When you're pregnant, even a simple headache or fever can feel like a high-stakes decision. You don't want to suffer, but you also don't want to risk your baby's health. That’s why so many people freeze up when they reach for the medicine cabinet. The truth? Not all pain relievers are created equal during pregnancy. Acetaminophen is still the go-to choice for most pregnant people - but NSAIDs like ibuprofen and naproxen? Those come with serious warnings, especially after 20 weeks.
Acetaminophen: The Only Over-the-Counter Pain Reliever Safe All Through Pregnancy
Acetaminophen, also known as paracetamol, has been used safely in pregnancy for over 70 years. It’s the active ingredient in Tylenol, Panadol, and many generic brands. Unlike aspirin or ibuprofen, it doesn’t affect blood clotting or reduce inflammation - it just takes away pain and lowers fever. That’s why doctors recommend it for everything from backaches to sinus infections to high fevers.
Large studies tracking tens of thousands of pregnancies have found no link between acetaminophen use and birth defects, preterm birth, or low birth weight. A major 2023 study in JAMA Network Open followed 97,000 mother-child pairs and found no increased risk of autism, ADHD, or intellectual disability in children whose mothers took acetaminophen during pregnancy. The adjusted odds ratios were nearly 1.0 - meaning no real difference from those who didn’t take it.
Even when it comes to fever, acetaminophen isn’t just helpful - it’s protective. A fever above 102°F in the first trimester can raise the risk of neural tube defects by up to 2.3 times. A 2019 study in Epidemiology showed that untreated fever during pregnancy increases miscarriage risk by 1.5 times. Taking acetaminophen to bring that fever down isn’t risky - it’s essential.
The standard dose is 325 to 1,000 mg every 4 to 6 hours, not to exceed 4,000 mg in a day. Most people find 500 mg every 6 hours is enough. Don’t take it longer than 3 to 5 days in a row without checking in with your provider. And yes - even if you’re in your third trimester, it’s still safe. The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine both reaffirmed this in 2025.
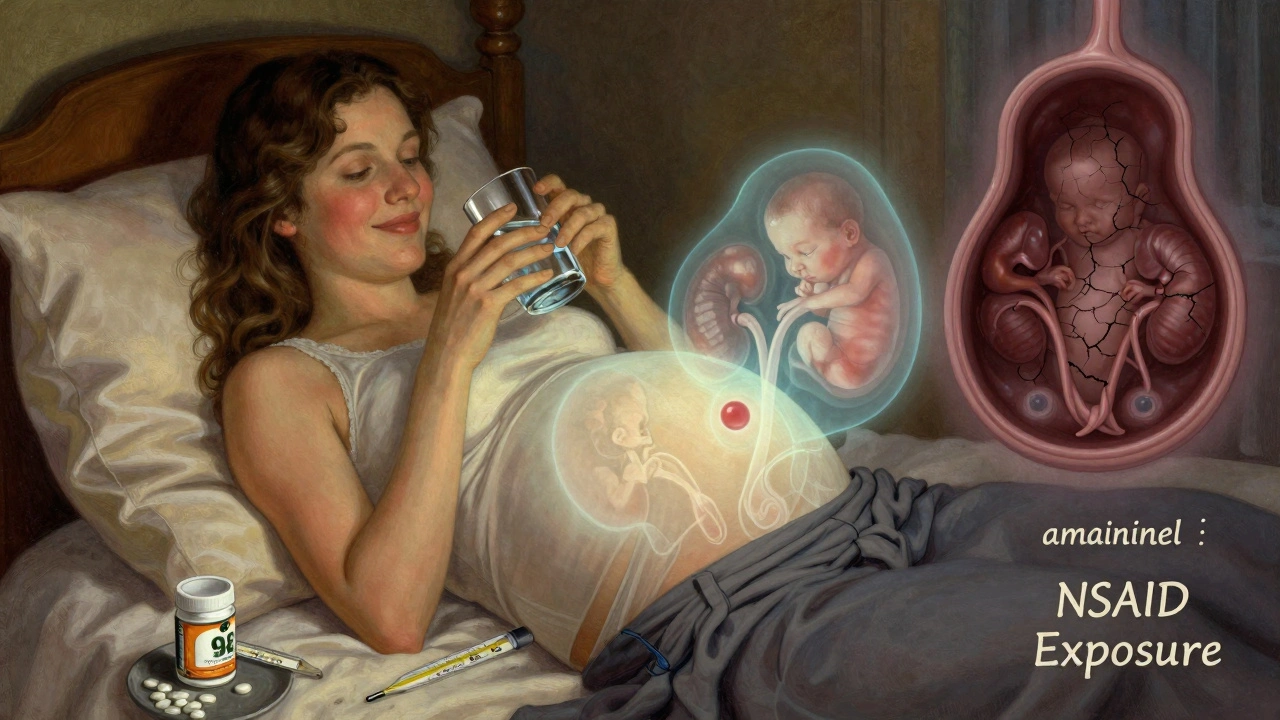
NSAIDs: The Hidden Danger After 20 Weeks
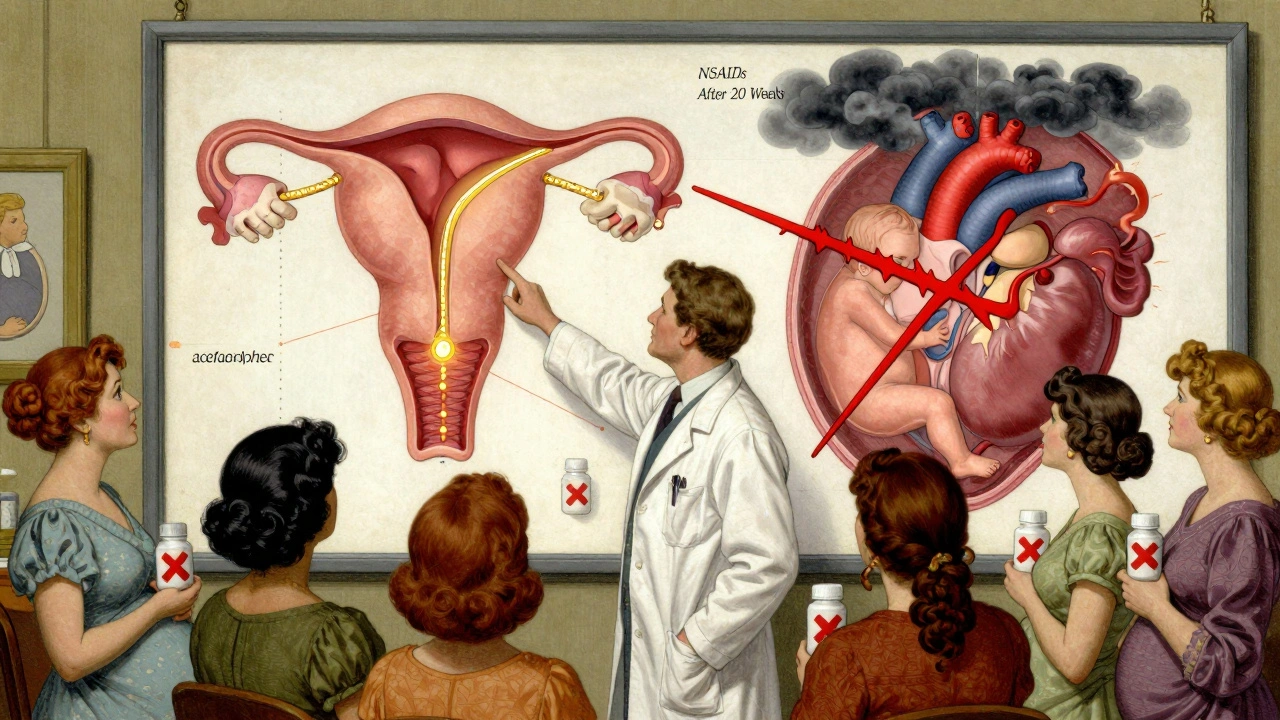
NSAIDs - nonsteroidal anti-inflammatory drugs - include ibuprofen (Advil, Motrin), naproxen (Aleve), diclofenac (Voltaren), and others. They’re great for swelling and inflammation, but they’re not safe for your baby after 20 weeks of pregnancy.
The FDA updated its warning in October 2020: NSAIDs must now carry labels saying they can cause serious kidney problems in the unborn baby starting at 20 weeks. That’s a big change from the old rule, which only warned against use after 30 weeks. Why the shift? Because research showed fetal kidneys start shutting down as early as 20 weeks when exposed to these drugs.
How does this happen? NSAIDs block enzymes that help produce amniotic fluid. Without enough fluid, the baby’s lungs can’t develop properly, and their kidneys struggle to function. Within 48 to 72 hours of taking an NSAID after 20 weeks, amniotic fluid levels can drop sharply - a condition called oligohydramnios. One study found this occurred in 1.2% of fetuses exposed to NSAIDs after 20 weeks, compared to just 0.1% in unexposed pregnancies.
After 30 weeks, there’s another risk: the fetal ductus arteriosus - a vital blood vessel that bypasses the lungs before birth - can close too early. This forces the baby’s heart to work harder and can lead to life-threatening complications. The risk is small - about 0.5% to 1% - but it’s real.
And here’s the catch: you might not even know you’re taking NSAIDs. About 30% of cold, flu, and sinus medications contain them. Read the Drug Facts label. Look for “ibuprofen,” “naproxen,” “ketoprofen,” or “indomethacin.” If you see it, put it back.
What About Before 20 Weeks? Can I Take NSAIDs Then?
Technically, NSAIDs are not banned before 20 weeks - but they’re still not recommended. The FDA’s 2020 warning didn’t say they’re safe before then. It just said the biggest dangers start at 20 weeks. That doesn’t mean they’re harmless earlier.
Some studies suggest NSAID use in the first trimester may slightly increase the risk of miscarriage. Others link them to a higher chance of congenital heart defects, though the evidence isn’t strong enough to be conclusive. The safest approach? Avoid them entirely unless your doctor says otherwise.
There’s one exception: low-dose aspirin (81 mg). If you’re at risk for preeclampsia, your provider may prescribe it. That’s not an NSAID in the same category as ibuprofen - it’s used for its blood-thinning effect, not pain relief. Don’t confuse it with regular aspirin.
Why So Much Confusion Among Pregnant People?
Despite clear guidelines, most pregnant people are scared to take any medicine. A 2023 survey of 1,200 pregnant patients found 68% avoided all pain relievers - and 42% specifically avoided acetaminophen because of rumors about autism.
Those rumors come from studies that show a statistical association - not causation. Just because some children with autism had mothers who took acetaminophen doesn’t mean the drug caused it. The same studies found no link when researchers controlled for other factors like maternal illness, fever, or genetic risks.
Dr. Salena Zanotti from Cleveland Clinic puts it plainly: “Acetaminophen is still the safest known drug to take during pregnancy for problems like fever and pain. It’s OK to turn to medication for help when symptoms are making your daily life difficult.”
Meanwhile, misinformation spreads fast on social media. Reddit threads, Instagram posts, and Facebook groups often highlight single studies out of context. One 2021 consensus paper in Nature Reviews Endocrinology raised theoretical concerns about endocrine disruption - but it didn’t prove harm. It just said, “Maybe we should study this more.” That got twisted into “Acetaminophen causes autism.”
Doctors are seeing the fallout. A 2022 AMA survey showed a 45% jump in patient questions about acetaminophen safety after that paper came out. Many patients stop taking it - even when they have a 103°F fever - because they’re afraid.
What Should You Do If You’ve Already Taken NSAIDs?
If you took ibuprofen or naproxen before you knew you were pregnant - don’t panic. Most early exposures don’t cause problems. But if you took them after 20 weeks, talk to your provider. They may recommend an ultrasound to check amniotic fluid levels.
If you’re between 20 and 30 weeks and took NSAIDs for more than 48 hours, your provider will likely monitor you closely. Oligohydramnios can often be reversed by stopping the drug and increasing fluids. But if fluid levels stay low, it can lead to complications.
Don’t wait until your next appointment. Call your OB or midwife right away if you’ve taken an NSAID after 20 weeks and feel less movement, or if you notice less frequent urination.
Practical Tips for Safe Pain Relief During Pregnancy
- Use acetaminophen (Tylenol) as your first choice for headaches, muscle aches, fever, or tooth pain - even in the third trimester.
- Stick to the lowest effective dose: 500 mg every 6 hours is usually enough.
- Don’t take it longer than 3-5 days in a row without checking in with your provider.
- Always read the Drug Facts label on cold, flu, and multi-symptom products. Avoid any with ibuprofen, naproxen, or aspirin (unless it’s 81 mg and prescribed).
- Try non-drug options too: warm compresses, rest, hydration, gentle stretching, or prenatal yoga for back pain.
- If you’re unsure whether a medication is safe, ask your pharmacist or provider. Don’t guess.
What’s Next? Research Is Still Evolving
The science isn’t frozen. The NIH is running the Acetaminophen Birth Cohort Study - tracking 10,000 pregnant women and their children through 2027 to see if long-term use affects brain development. Some early data suggest chronic, high-dose use might carry small risks, but nothing that outweighs the dangers of untreated fever or pain.
Researchers are also looking at genetics. A 2024 study found that 15% of pregnant women have a gene variant (CYP2E1) that affects how their body breaks down acetaminophen. That could mean some people are more sensitive to side effects - but we don’t yet know how to use that info in practice.
For now, the message is clear: if you need pain relief during pregnancy, acetaminophen is your safest bet. NSAIDs? Avoid them after 20 weeks. And if you’re unsure - ask. Your provider is there to help you make the right call, not judge you for needing help.
Is acetaminophen safe during all three trimesters of pregnancy?
Yes, acetaminophen is considered safe for use throughout all trimesters of pregnancy when taken at recommended doses (325-1,000 mg per dose, up to 4,000 mg daily). Major medical organizations, including ACOG and SMFM, confirm its safety based on decades of research. It’s the only over-the-counter pain reliever with this level of support for use in pregnancy.
Can I take ibuprofen in the first trimester?
While ibuprofen is not officially banned before 20 weeks, it’s still not recommended. Some studies suggest a possible link to early miscarriage or heart defects, though the evidence is limited. The safest choice is to avoid NSAIDs entirely and use acetaminophen instead. If you accidentally took ibuprofen early on, don’t panic - but talk to your provider about it.
What happens if I take NSAIDs after 20 weeks?
Taking NSAIDs after 20 weeks can cause fetal kidney problems, leading to low amniotic fluid (oligohydramnios). This can affect lung development and increase the risk of complications. In rare cases, it can also cause early closure of a critical blood vessel in the baby’s heart. If you took NSAIDs after 20 weeks, contact your provider. An ultrasound can check amniotic fluid levels, and stopping the drug often reverses the issue.
Does acetaminophen cause autism or ADHD in children?
No. A large 2023 study of over 97,000 mother-child pairs found no increased risk of autism, ADHD, or intellectual disability linked to acetaminophen use during pregnancy. Some earlier studies suggested a connection, but they didn’t account for other factors like maternal illness or fever. When those are controlled for, the link disappears. Experts agree the benefits of treating fever and pain far outweigh any theoretical risks.
Are there any safe alternatives to acetaminophen for pain relief during pregnancy?
Yes - but not other pills. Non-medication options like heat packs, massage, prenatal yoga, acupuncture, and rest are safe and effective for many types of pain. For headaches, staying hydrated and managing stress helps. For back pain, supportive maternity belts and physical therapy can make a big difference. If you need medicine, acetaminophen is still the only recommended oral option.
Can I take cold and flu medicine while pregnant?
Only if it contains acetaminophen and no NSAIDs or decongestants like pseudoephedrine. Many multi-symptom cold medicines include ibuprofen, naproxen, or phenylephrine - all of which are risky during pregnancy. Always check the Drug Facts label. If you’re unsure, ask your pharmacist or provider. Stick to single-ingredient products when possible.


Write a comment