Drinking alcohol with diabetes isn’t just about counting carbs-it’s about staying alive. For many people with diabetes, alcohol feels like a harmless social habit. But behind that glass of wine or beer is a silent threat: hypoglycemia. It can sneak up hours after you’ve finished drinking, even while you’re asleep. And because the symptoms-dizziness, confusion, sweating-look exactly like being drunk, no one may realize you’re in a medical emergency.
How Alcohol Messes With Your Blood Sugar
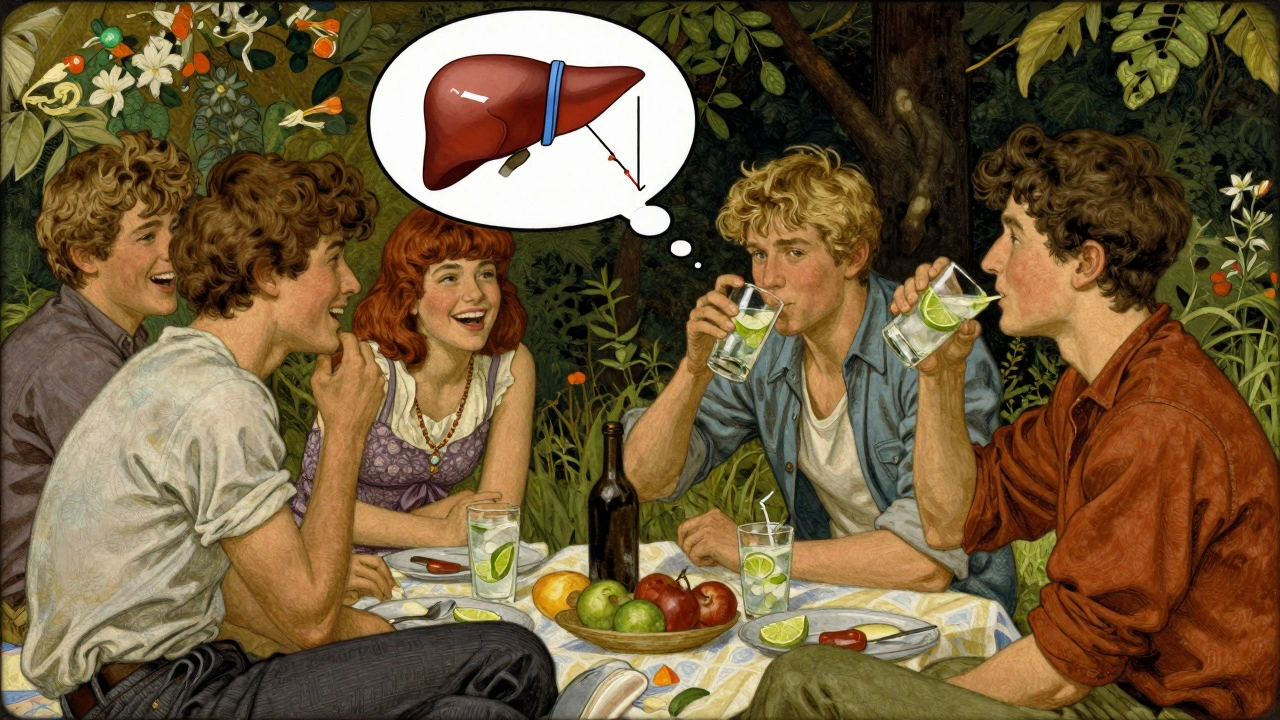
Alcohol doesn’t just raise or lower blood sugar-it flips the script. When you drink, your liver stops making glucose. That’s its normal job: keeping your blood sugar steady between meals or overnight. But when alcohol is in your system, the liver treats it like a toxin and focuses on clearing it out. That means no glucose production. Meanwhile, if you’re taking insulin or sulfonylureas, your body is still pushing glucose into your cells. The result? A dangerous drop in blood sugar that can last up to 12 hours.
This isn’t theoretical. Research from Mount Sinai shows hypoglycemia risk spikes within 30 minutes of drinking and doesn’t fade until the alcohol is fully processed. For people with type 1 diabetes, about 30% experience at least one severe low after drinking, according to Breakthrough T1D. Even one drink can trigger it if you haven’t eaten or if you’re active.
What Counts as a Standard Drink?
Not all drinks are equal. A “drink” in medical terms isn’t what you pour at home-it’s a fixed amount:
- 12 oz (360 mL) of regular beer (5% alcohol)
- 5 oz (150 mL) of wine (12% alcohol)
- 1.5 oz (45 mL) of hard liquor (80 proof, 40% alcohol)
That’s it. Anything more increases your risk. The American Diabetes Association and Diabetes UK agree: women should stick to one drink per day, men to two. But here’s the catch-those limits are only safe if you’re not skipping meals, not exercising, and not on certain medications.
Some drinks marketed as “diabetic-friendly” are traps. Low-sugar beers and ciders often have higher alcohol content-sometimes 2-3% more than regular versions. That means more liver stress, more glucose suppression, and a higher chance of a late-night hypo. Skip them.
Which Drinks Are Safest?
Not all alcohol is created equal when it comes to blood sugar. Here’s what works:
- Dry red or white wine (under 4g carbs per 5 oz serving)
- Light beer (under 5g carbs per 12 oz)
- Hard seltzers (3-4g carbs per can)
- Spirits like vodka, gin, or whiskey mixed with club soda or diet tonic
These options have minimal sugar and carbs. But here’s the kicker: even these can cause lows if you drink on an empty stomach. The key isn’t just what you drink-it’s how you drink it.
On the other end, avoid anything sweet:
- Margaritas (up to 25g carbs)
- Sweet wines (Port, Sherry, Moscato)
- Liqueurs (Baileys, Kahlua)
- Cocktails with regular soda, juice, or syrup
Diabetes UK found drinks with 10g+ carbs per serving raise blood sugar spikes by 35%, followed by crashing lows later. That rollercoaster is dangerous.
When Not to Drink at All
Some situations make alcohol too risky to even consider:
- Your blood sugar is below 100 mg/dL or above 300 mg/dL
- You’ve exercised in the last 2 hours
- You’re pregnant
- You have diabetic neuropathy, pancreatitis, or liver disease
WebMD and MedlinePlus both say: if your blood sugar is already low or unstable, don’t drink. Exercise and alcohol together? That’s a double hit. Your muscles use glucose, and your liver can’t replace it. Studies show this combo increases hypoglycemia risk by 40%.
And if you’re on sulfonylureas (like glipizide or glyburide), alcohol raises your hypo risk by 50%. Metformin users should avoid heavy drinking-more than four drinks in two hours can trigger lactic acidosis, a rare but life-threatening condition.
The Safe Drinking Protocol
If you choose to drink, follow this step-by-step plan:
- Check your blood sugar before you start. Target: 100-140 mg/dL.
- Eat a meal with 15-30g of carbs. No exceptions. Pizza, pasta, rice, or even a sandwich works.
- Drink slowly. Space drinks out over hours, not shots in 20 minutes.
- Check your blood sugar every 2 hours while drinking.
- Check again before bed-even if you feel fine. Set an alarm if needed.
- Have fast-acting glucose on hand: 15g of glucose tablets, juice, or candy.
- Wear medical alert jewelry. If you pass out, someone needs to know you have diabetes.
This isn’t optional. People on Reddit’s r/diabetes community who followed this routine reported 82% fewer hypos. Those who skipped meals or didn’t check after drinking? Most had emergencies.
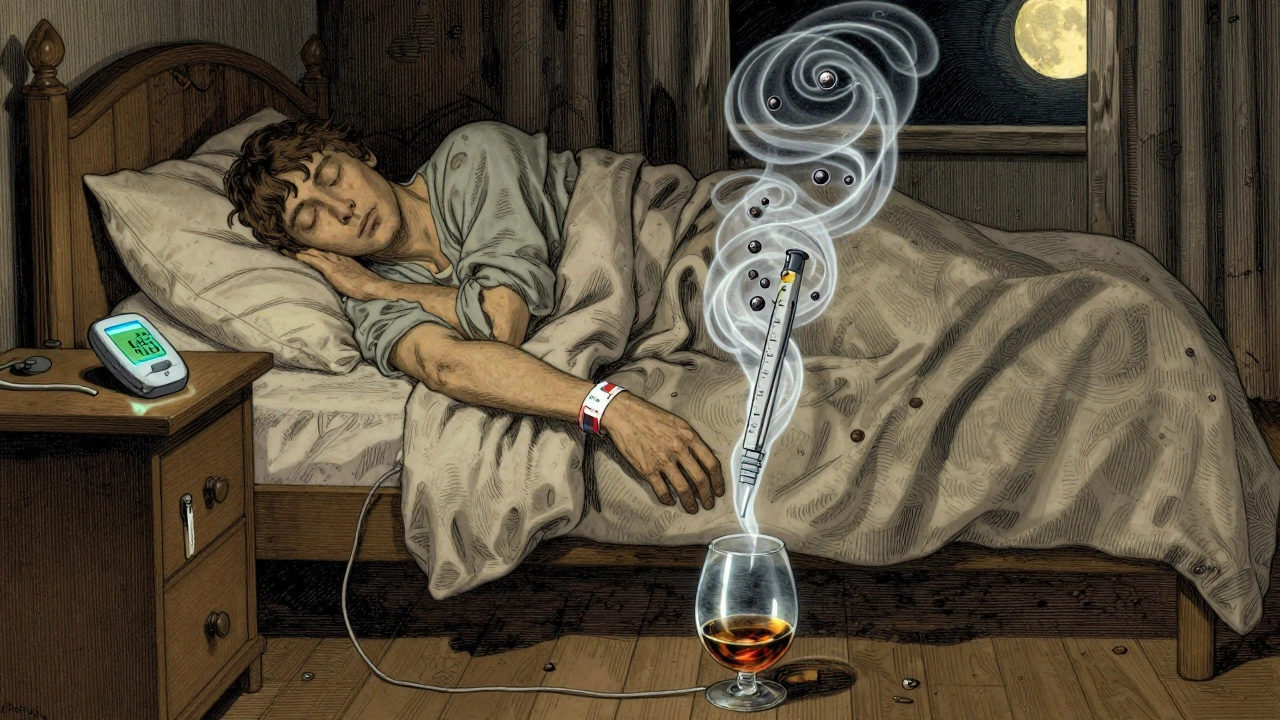
Why Nighttime Hypos Are the Most Dangerous
The biggest danger isn’t during the party-it’s at 3 a.m. Alcohol delays the drop in blood sugar. You might go to bed feeling fine, but your liver is still busy processing booze. By morning, your glucose is plummeting.
Sixty-one percent of alcohol-related diabetes emergencies happen overnight, according to user reports on Breakthrough T1D forums. That’s why checking before bed is non-negotiable. If your sugar is below 100 mg/dL, eat a small snack with carbs and protein-like a piece of toast with peanut butter. It gives your liver something to work with while it’s still clearing alcohol.
And here’s the scary part: your body’s warning signs for low blood sugar-shaking, sweating, hunger-get masked by alcohol. You might feel dizzy and think, “I had too much to drink,” when you’re actually in danger. That’s why wearing a medical alert bracelet isn’t just smart-it’s life-saving.
New Tech Is Helping, But It’s Not a Substitute
Technology is catching up. The Dexcom G7 CGM now includes an “Alcohol-Diabetes Safety Algorithm” that flags rising hypo risk during and after drinking. In trials, it cut severe events by 37%. That’s huge.
But don’t rely on it. Algorithms can’t replace your judgment. You still need to eat, check, and monitor. The ADA’s 2024 draft guidelines are moving toward personalized thresholds based on your CGM data, not fixed numbers. That’s good news-but it’s still in testing.
Right now, the safest strategy is simple: eat, check, drink slowly, check again, and never drink alone.
Is Any Alcohol Worth It?
Some studies suggest moderate red wine might improve insulin sensitivity by 12% in type 2 diabetes. Others say light drinking lowers heart disease risk by 15-20%. But the American Diabetes Association is clear: no one should start drinking for health reasons.
If you already drink, you can do it safely. But if you don’t drink, don’t start. The risks outweigh any potential benefit.
Alcohol isn’t the enemy. But it’s a powerful tool that can turn against you if you don’t respect it. For people with diabetes, drinking isn’t about choice-it’s about control. Control your intake. Control your timing. Control your snacks. And above all, control your expectations. One drink can cost you more than a bad hangover. It can cost you your health.
Can I drink alcohol if I have type 1 diabetes?
Yes, but with extreme caution. People with type 1 diabetes are at higher risk of alcohol-induced hypoglycemia because their bodies don’t naturally regulate blood sugar. Always eat carbs before drinking, check your glucose before, during, and after, and never drink without someone nearby who knows you have diabetes. Keep fast-acting glucose handy at all times.
Why does alcohol cause low blood sugar hours later?
Your liver prioritizes breaking down alcohol over releasing glucose. This suppression of glucose production can last 8-12 hours after your last drink. If you’re on insulin or similar medications, your body keeps using glucose, but your liver isn’t replacing it. That’s why lows often hit overnight or the next morning.
Is wine safer than beer for people with diabetes?
Dry wine is generally safer than beer because it has fewer carbs-about 0-4g per 5 oz glass. Regular beer can have 10-15g carbs per 12 oz. But alcohol content matters too. High-alcohol wines (above 12%) suppress glucose production more, so even dry wine can be risky if consumed in excess. Stick to one glass and always eat with it.
Can I drink alcohol if I’m on metformin?
Moderate drinking (1-2 drinks) is usually safe with metformin, but heavy drinking (more than 4 drinks in 2 hours) increases the risk of lactic acidosis-a rare but serious condition. Avoid binge drinking. Always stay hydrated and never drink on an empty stomach.
What should I do if I feel dizzy after drinking?
Don’t assume it’s just being drunk. Check your blood sugar immediately. If it’s below 70 mg/dL, consume 15g of fast-acting glucose (glucose tablets, juice, or candy). Wait 15 minutes and check again. If it doesn’t rise, repeat. If you’re confused or can’t check yourself, call for help. Tell someone you have diabetes-your symptoms could be mistaken for intoxication.
Should I avoid alcohol if I have nerve damage from diabetes?
Yes. If you have diabetic neuropathy, alcohol can make nerve damage worse. It’s toxic to nerves and can increase pain, tingling, and numbness. MedlinePlus and the ADA both recommend complete avoidance. There’s no safe level if your nerves are already damaged.
Are sugar-free cocktails safe for people with diabetes?
Only if the mixer is truly sugar-free. Diet tonic, club soda, or plain water are fine. But many “sugar-free” cocktails still contain hidden carbs from flavorings or liqueurs. Always check labels. A vodka soda with lime is safe. A “sugar-free margarita” might not be. When in doubt, stick to plain spirits with water.
Can I drink alcohol after exercising?
No. Exercise already lowers blood sugar. Alcohol suppresses glucose production. Together, they create a perfect storm for severe hypoglycemia. Wait at least 2 hours after exercise before drinking-and even then, eat carbs and check your levels before you start.


Write a comment