Every year, millions of people reach for antihistamines and decongestants to chase away sneezing, runny noses, and stuffy sinuses. These medications are on every pharmacy shelf, sold without a prescription, and often treated like candy-quick fixes you grab without a second thought. But here’s the truth: antihistamines and decongestants aren’t harmless. They carry real, sometimes dangerous risks that most users never consider until it’s too late.
What Antihistamines Actually Do (And Why They Can Hurt You)
Antihistamines block histamine, the chemical your body releases during an allergic reaction. That’s why they stop itching, sneezing, and watery eyes. But not all antihistamines are the same. The older ones-like diphenhydramine (Benadryl) and doxylamine (Unisom)-cross into your brain and mess with your nervous system. That’s why you get sleepy. About 60% of people using these first-generation drugs feel drowsy, dizzy, or foggy. For some, it’s worse: blurry vision, dry mouth, constipation, trouble peeing, or even confusion.
That’s not just annoying. It’s dangerous. In people over 65, these drugs can increase the risk of falling by 300%. That’s not a typo. One study found that nearly 1 in 3 older adults who took diphenhydramine had a fall within a month. Many ended up in the hospital with broken hips or head injuries. The American Geriatrics Society lists these drugs as potentially inappropriate for seniors because they mimic the effects of dementia-slowing thinking, blurring vision, and making you unsteady.
Even worse, they can make sinus infections worse. When antihistamines dry up mucus, they don’t just stop the runny nose-they trap gunk inside your sinuses. That thick, sticky mucus becomes a breeding ground for bacteria. One doctor found that 25% of patients who used antihistamines long-term ended up with bacterial sinus infections they didn’t have before.
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are much safer. They barely enter the brain, so drowsiness drops to 10-15%. But they’re not risk-free. People with glaucoma, enlarged prostates, or liver disease can still have bad reactions. And if you’re on antidepressants or other meds, the interactions can be serious.
Decongestants: The Hidden Blood Pressure Bomb
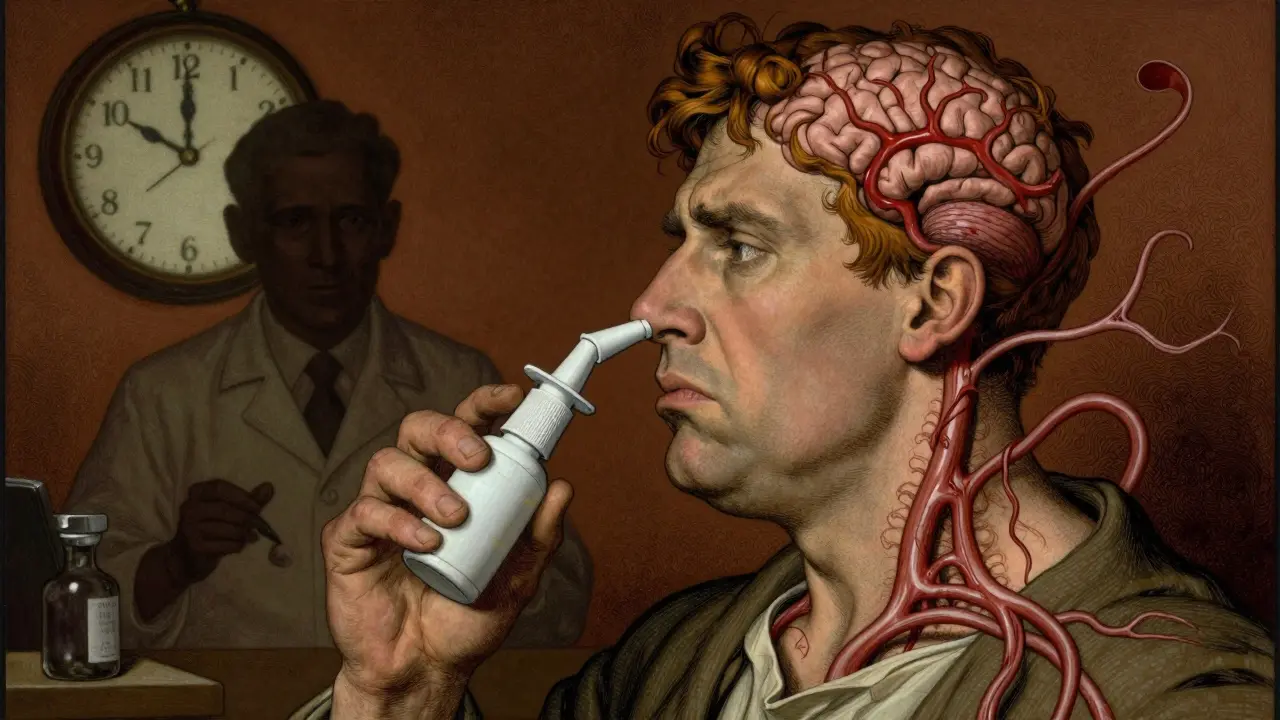
Decongestants like pseudoephedrine (Sudafed) and phenylephrine work by shrinking swollen blood vessels in your nose. That’s why your nose clears up in minutes. But that same vasoconstriction happens everywhere-in your heart, your brain, your kidneys. And that’s where the danger lies.
Even a healthy person can see their blood pressure rise by 5-10 mmHg after taking a decongestant. For someone with high blood pressure-116 million Americans-that’s enough to trigger a stroke or heart attack. The Mayo Clinic says decongestants can be more harmful than helpful for people with heart disease, thyroid problems, or diabetes. And if you’re on an MAOI antidepressant? That combo can cause a life-threatening spike in blood pressure, sometimes over 180 mmHg.
And don’t think nasal sprays are safer. Oxymetazoline (Afrin) gives fast relief, but if you use it longer than three days, you get rebound congestion. That’s when your nose gets even more swollen than before. Half the people who use these sprays past the limit end up dependent on them. They can’t breathe without the spray, so they use more-and the cycle gets worse.
And yes, it gets weirder. A tiny number of people-about 1 in 2,000-report hallucinations or severe anxiety after taking decongestants. Not because they’re “crazy.” Because the drug is overstimulating their nervous system. It’s rare, but it’s real.
Combination Products: The Silent Overdose Risk
Most people don’t realize that “all-in-one” cold and allergy meds are loaded with multiple drugs. One pill might contain an antihistamine, a decongestant, and acetaminophen (Tylenol). That sounds convenient. Until you take another Tylenol for a headache, or drink alcohol, or forget you already took it.
Acetaminophen overdose is the #1 cause of acute liver failure in the U.S. The safe daily limit is 4,000 mg. But many combination products have 500-650 mg per tablet. It’s easy to hit 5,000 mg without meaning to. And once your liver starts failing, there’s no warning-no pain, no nausea-until it’s too late.
And then there’s the antihistamine. If you have an enlarged prostate, taking it can lock your bladder shut. You can’t pee. You need a catheter. That’s not rare. Emergency rooms see this every week, especially in older men who think “it’s just a cold pill.”
Who Should Never Take These Meds (Without a Doctor)
You don’t need to be a medical expert to know if you’re at risk. Here’s who should avoid these drugs entirely-or at least talk to a doctor first:
- Anyone with high blood pressure
- People with heart disease, irregular heartbeat, or history of stroke
- Men with enlarged prostates
- People with glaucoma (especially angle-closure)
- Those with thyroid problems
- Anyone with liver or kidney disease
- People on antidepressants, especially MAOIs or SSRIs
- Pregnant women in the first trimester
- Children under 2 years old
- Adults over 65
The NHS and FDA both say: if you have any of these conditions, don’t guess. Don’t assume “it’s just OTC.” Ask your doctor. Or better yet, talk to your pharmacist. They see these mistakes every day.
What You’re Not Thinking About: Drug Interactions
Most people check for food interactions. Few check for drug interactions. But OTC meds don’t play nice with other substances.
Alcohol + antihistamine = doubled drowsiness. That’s why so many older adults fall after having a glass of wine with their Benadryl. Energy drinks + decongestants = racing heart, panic attacks, even seizures. One poison control center saw a 25% jump in calls from young adults mixing Sudafed with caffeine-heavy drinks.
Even common supplements like St. John’s Wort or ginseng can interact. So can herbal teas. And if you’re on blood thinners, antihistamines can increase bleeding risk. The list goes on.
There’s no app that tells you every possible interaction. That’s why pharmacists exist. Walk into a pharmacy and ask: “I’m taking this. What shouldn’t I mix it with?”

When to Stop and See a Doctor
Allergies usually last a week or two. If your symptoms are still going after 10-14 days, you’re not dealing with allergies anymore. You might have a sinus infection, a cold that turned bacterial, or something else entirely.
Using decongestants or antihistamines past that point doesn’t help. It just masks the real problem. And the longer you wait, the worse it gets.
Also, if you start having new symptoms-chest pain, trouble breathing, confusion, vision changes, or inability to urinate-stop the meds. Right now. Go to a clinic. Don’t wait. Don’t think it’s “just a side effect.”
What to Use Instead
You don’t need to suffer. There are safer options.
- Saline nasal sprays: rinse out allergens without chemicals
- Intranasal corticosteroids (like Flonase): reduce inflammation long-term with almost no systemic side effects
- Allergy shots or tablets: for long-term relief, especially if you know your triggers
- Humidifiers: keep nasal passages moist, reduce irritation
- HEPA filters: remove allergens from your home air
These don’t work instantly. But they work without risking your heart, liver, or brain.
Bottom Line: OTC Doesn’t Mean Safe
Just because you can buy it off the shelf doesn’t mean it’s harmless. Antihistamines and decongestants are powerful drugs with serious side effects. They’re not candy. They’re not harmless fixes. They’re chemicals that alter your body’s chemistry-and they can hurt you if you don’t treat them with respect.
Before you take one, ask yourself:
- Do I have high blood pressure, heart disease, or an enlarged prostate?
- Am I over 65?
- Am I taking any other meds or supplements?
- Have I used this for more than 3 days?
- Is this really helping-or just masking something worse?
If you answered yes to any of these, talk to a doctor or pharmacist before taking another pill. Your body isn’t a lab experiment. Don’t gamble with your health just because the medicine is cheap and easy to get.
Can antihistamines cause dementia?
Long-term use of first-generation antihistamines like diphenhydramine has been linked to higher dementia risk in older adults. These drugs block acetylcholine, a brain chemical critical for memory and thinking. Studies show people who take them daily for years have a 50% higher chance of developing dementia. Switching to second-generation antihistamines like loratadine reduces this risk significantly.
Is it safe to take decongestants if I have high blood pressure?
No. Decongestants like pseudoephedrine and phenylephrine raise blood pressure by narrowing blood vessels. Even if your blood pressure is controlled, these meds can push it into dangerous territory. The FDA and Mayo Clinic both warn against their use in people with hypertension. Safer alternatives include saline sprays, humidifiers, or intranasal corticosteroids.
Why can’t kids under 2 have allergy meds?
The FDA banned OTC cough and cold medicines for children under 2 after 123 cases of serious side effects-including seizures, rapid heart rate, and death-were reported between 1969 and 2006. Their bodies process these drugs differently, and even small doses can be toxic. For infants with congestion, use saline drops and a bulb syringe instead.
Can I take antihistamines with alcohol?
No. Alcohol makes antihistamines much stronger. Together, they cause extreme drowsiness, dizziness, and poor coordination. In older adults, this combo increases fall risk by 50%. It can also impair judgment and reaction time, making driving or operating machinery dangerous. Even one drink with Benadryl can be risky.
How long is it safe to use nasal decongestant sprays?
No longer than 3 days. Using sprays like Afrin past that point causes rebound congestion-your nose becomes more swollen than before. This leads to dependency, where you need more spray just to breathe. About half of users who go beyond 3 days develop this condition. Stick to saline sprays or oral options if you need longer relief.
Are second-generation antihistamines completely safe?
They’re much safer than first-gen options, but not risk-free. People with liver disease, kidney problems, or glaucoma should still check with a doctor. Some, like cetirizine, can still cause drowsiness in sensitive individuals. And they can interact with other meds. Always read the label and ask your pharmacist if you’re unsure.
If you’re using OTC allergy meds regularly, you’re not alone-but you’re also not safe. These drugs are powerful, and their risks are hidden in plain sight. Talk to your doctor before the next sneeze turns into a crisis.


Write a comment