Alzheimer’s disease doesn’t start with forgetting where you put your keys. It begins quietly - a name slips away, a conversation is repeated, a familiar street feels strange. By the time families notice, the brain has already been changing for years. This isn’t just aging. It’s a biological storm inside the skull, slowly erasing memories, identity, and independence. And behind every person with Alzheimer’s is someone else - a spouse, a child, a friend - holding on as everything shifts.
What Happens in the Brain?
Alzheimer’s isn’t one thing. It’s two tangled messes in the brain: sticky plaques made of amyloid-beta proteins, and twisted fibers of tau protein called neurofibrillary tangles. These aren’t just annoyances. They choke the connections between brain cells, especially in the hippocampus - the area that turns short-term memories into long-term ones. As those connections die, the brain shrinks. The person doesn’t forget because they’re lazy or distracted. Their brain literally can’t hold onto new information anymore.
By the time symptoms show up, the damage has been building for 15 to 20 years. That’s why early detection matters. Blood tests are coming that can spot these changes before memory problems start. In 2023, the FDA approved lecanemab, the first drug that actually slows the buildup of amyloid plaques. It doesn’t cure Alzheimer’s, but in clinical trials, it cut cognitive decline by 27% over 18 months. It’s not for everyone - it requires monthly infusions and regular brain scans to watch for side effects - but it’s proof that targeting the biology works.
The Stages: From Subtle Lapses to Total Dependence
Alzheimer’s doesn’t jump from sharp to lost. It creeps. Experts break it into stages to help families prepare, but no two people follow the same path. Some decline fast. Others live for two decades after diagnosis.
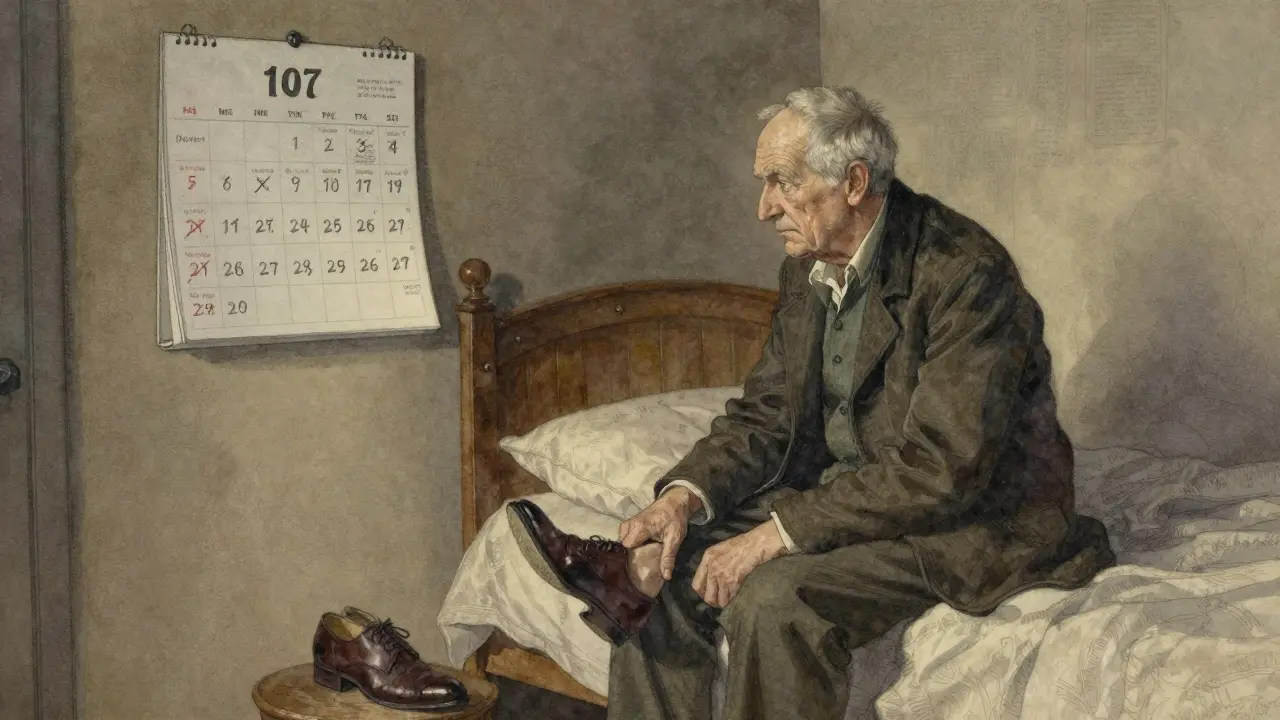
Early Stage (Mild): This is when people still drive, cook, and pay bills - but not quite like before. They forget recent conversations, repeat questions, misplace things like glasses or keys, and struggle to find the right word. They might get anxious or withdrawn. At this point, they know something’s wrong. They hide it. They make lists. They set alarms. They rely on calendars, labeled cabinets, and reminder apps. A simple test: if someone can’t remember three words after five minutes, even with cues, it’s a red flag.
Middle Stage (Moderate): This is the longest phase - often lasting years. The person forgets their own address, gets lost in their own neighborhood, and can’t dress themselves. They might accuse caregivers of stealing, hide things, or wander at night. Bathing and toileting become battles. Repetitive behaviors - hand-wringing, pacing, asking the same question 20 times - are common. Sleep flips. They sleep all day and are awake all night. This stage is emotionally brutal for caregivers. The person isn’t being difficult. Their brain has lost the ability to filter thoughts, control impulses, or understand reality. A 2022 survey found 78% of caregivers felt intense anxiety during this phase because of behavioral changes.
Late Stage (Severe): The brain is severely damaged. The person can’t speak, recognize loved ones, or control movement. They may be bedbound. Swallowing becomes dangerous - food or saliva can enter the lungs, leading to pneumonia, which is the most common cause of death. They can’t tell you they’re in pain. They don’t respond to words. But they still respond to touch. A gentle hand on the arm. A familiar song. A soft voice. These moments matter more than ever. Care is now 24/7. Every need - eating, turning in bed, cleaning - requires help. The emotional toll shifts. Many caregivers say this stage is physically exhausting but less emotionally chaotic than the middle stage.

Memory Loss: It’s Not Just Forgetting
Not all memory loss is Alzheimer’s. Normal aging means you forget where you put your keys. Alzheimer’s means you forget what keys are for. In early Alzheimer’s, only recent memories fade. Long-term memories - childhood, first job, wedding - stay intact longer. That’s why someone might not remember your name but can tell you exactly how they made apple pie in 1962.
Formal testing shows clear patterns: people with Alzheimer’s struggle with word lists. They learn fewer words, forget them quickly, and don’t improve when given hints. They also start making up answers - saying they saw a word that wasn’t even on the list. That’s called a false positive intrusion. It’s not lying. Their brain is filling gaps because the real memory is gone.
And it’s not just memory. Executive function - planning, organizing, problem-solving - goes first. That’s why someone can’t balance a checkbook or follow a recipe anymore. They might dress in layers in summer or wear pajamas to the grocery store. It’s not laziness. It’s brain failure.
What Caregivers Need - And How to Get It
Over 11 million Americans are unpaid caregivers for someone with Alzheimer’s. They work 27 hours a week on average - more than a full-time job - and 39% say their emotional stress is high or very high. Many don’t ask for help. They feel guilty. Or they think no one else can do it.
Here’s what actually works:
- Early stage: Support independence. Use labels on drawers, digital reminders, and a daily routine. Keep the environment calm and familiar. Don’t correct them when they’re wrong. Say, “Let’s look at the calendar,” instead of “You just asked that.”
- Middle stage: Safety first. Install door alarms. Remove throw rugs. Lock up medications and sharp objects. Create a quiet space. Use simple, one-step instructions: “Time to wash your hands,” not “Could you please go to the bathroom and wash your hands with soap?” Validation therapy helps - accept their reality. If they think their dead spouse is in the room, don’t argue. Say, “Tell me about him.”
- Late stage: Comfort is everything. Keep skin clean and dry to prevent sores. Turn them every two hours. Use soft music or familiar voices. Hold their hand. Even if they don’t respond, they feel it. Pain management is critical - they can’t say they hurt.
Respite care is not a luxury. It’s survival. Medicare covers up to five days of inpatient respite care per benefit period for hospice-eligible patients. Local adult day centers offer supervised care for a few hours a day. Even one afternoon off can reset a caregiver’s mental health.

The Bigger Picture
Alzheimer’s isn’t just a family crisis. It’s a global one. Over 55 million people live with dementia worldwide. By 2050, that number will hit 139 million. In the U.S. alone, the cost hit $345 billion in 2023 - $155 billion paid by Medicare, $89 billion by Medicaid, and $340 billion from unpaid family care. That’s more than cancer and heart disease combined.
And yet, most people don’t know the difference between Alzheimer’s and other dementias. Frontotemporal dementia, for example, often starts with personality changes or language loss - not memory. That’s why misdiagnosis is common. Early and accurate diagnosis matters, not just for treatment, but for planning.
Research is moving fast. Blood tests for amyloid and tau are coming. Drugs targeting tau and brain inflammation are in late-stage trials. But progress won’t help if it’s only for the wealthy. Right now, biomarker tests cost $3,000 to $5,000 - out of reach for most families, especially outside the U.S.
What You Can Do Today
If you’re worried about yourself or someone you love:
- Track changes. Write down specific examples: “Forgot my daughter’s birthday,” “Got lost driving home from the store.”
- See a doctor. Don’t wait. A neurologist or geriatrician can run cognitive tests and rule out other causes like vitamin deficiency or thyroid issues.
- Connect with support. The Alzheimer’s Association has free 24/7 helplines and local caregiver groups. Reddit’s r/dementia community is full of real stories and practical tips.
- Plan ahead. Legal documents - power of attorney, advance directives - need to be signed while the person still understands them.
There’s no magic cure. But there’s power in knowing what’s coming. In understanding that the person isn’t being difficult - they’re losing their mind. And in realizing that caregivers aren’t alone. Help exists. It’s just not always easy to find.
Is memory loss always a sign of Alzheimer’s?
No. Memory lapses can come from stress, sleep problems, depression, vitamin B12 deficiency, thyroid issues, or even certain medications. Alzheimer’s is diagnosed by ruling out other causes and showing a specific pattern of cognitive decline - especially trouble with new memories, not just forgetting old ones. If memory loss is sudden or only affects one area like language or movement, it could be another type of dementia.
Can Alzheimer’s be prevented?
There’s no sure way to prevent it, but lifestyle choices can lower risk. Regular exercise, a heart-healthy diet (like the MIND diet), managing blood pressure and diabetes, staying socially active, and getting enough sleep all help. Smoking and heavy drinking increase risk. The brain is a muscle - keeping it active with puzzles, reading, or learning new skills may build resilience.
How long do people live after an Alzheimer’s diagnosis?
It varies widely. On average, people live 4 to 8 years after diagnosis, but some live up to 20 years. Age at diagnosis matters - those diagnosed in their 60s often live longer than those diagnosed in their 80s. The cause of death is usually a complication like pneumonia, infection, or blood clots, not Alzheimer’s itself.
What’s the difference between Alzheimer’s and dementia?
Dementia is a general term for memory loss and thinking problems severe enough to interfere with daily life. Alzheimer’s is the most common cause - it makes up 60 to 80% of cases. Other types include vascular dementia (from strokes), Lewy body dementia (with hallucinations and movement issues), and frontotemporal dementia (which affects behavior or language first). Each has different symptoms and brain changes.
Are there any new treatments on the horizon?
Yes. Lecanemab and donanemab are the first drugs that target the underlying cause - amyloid plaques - and slow decline. More drugs are in testing, including ones that target tau protein, brain inflammation, and metabolic problems. Blood tests to detect Alzheimer’s before symptoms appear are expected within five years. But access is a problem. These treatments are expensive, require frequent monitoring, and aren’t covered by all insurance plans.
How do I know when it’s time for professional care?
Signs include: constant supervision needed, frequent wandering or safety risks, inability to manage medications, incontinence, or caregiver burnout. If you’re exhausted, sick, or feeling resentful, it’s not weakness - it’s a signal. Professional care isn’t giving up. It’s making sure both the person with Alzheimer’s and the caregiver get the support they need to stay safe and healthy.

Write a comment