Cytokine Bone Health Calculator
Calculate your bone loss risk based on cytokine levels, vitamin D, exercise, and other factors. This tool helps you understand how inflammation affects bone health and what actions you can take to protect your bones.
Your Bone Health Risk Assessment
Key Findings
Recommendations
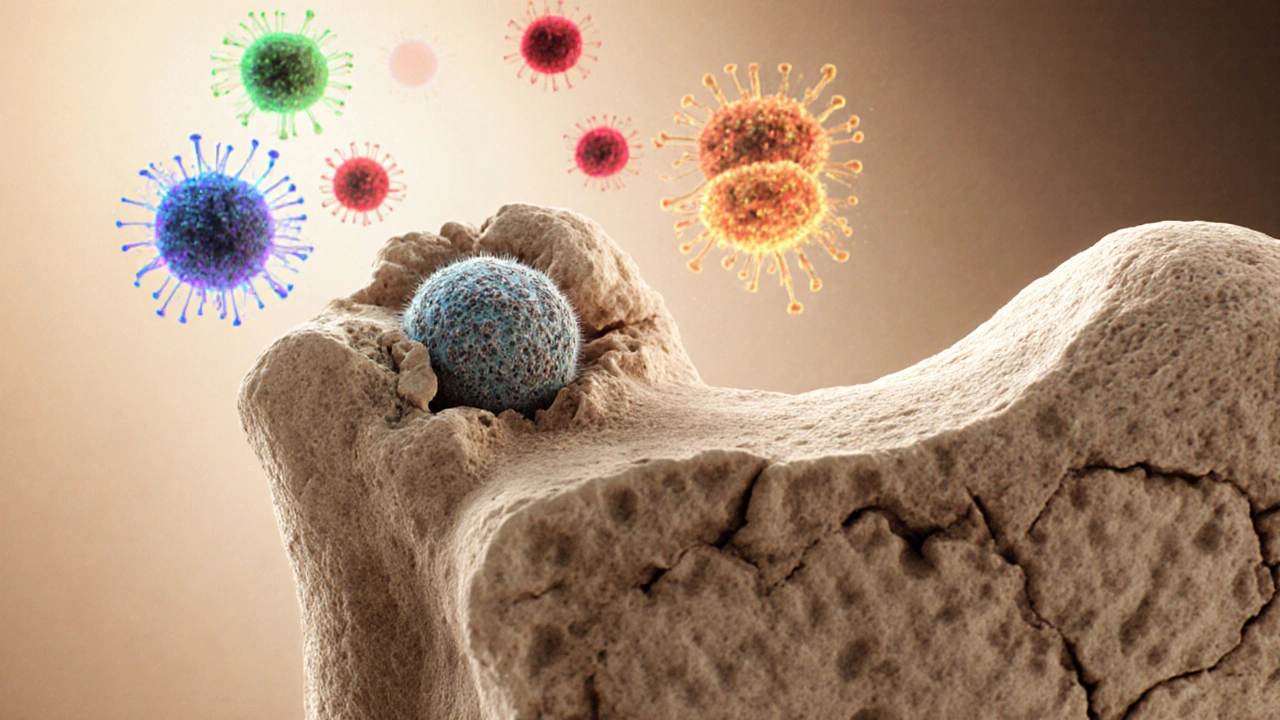
Ever wonder why a virus or chronic inflammation can leave you feeling achy and fragile? The answer lies in a hidden conversation between your bones and your immune system. When that dialogue gets out of sync, bone loss can accelerate - and the culprit isn’t always calcium.
Quick Takeaways
- Bone loss is driven by immune‑derived signals that tell osteoclasts to break down bone.
- Key cytokines such as RANKL, IL‑6, and TNF‑α act as messengers linking inflammation to bone erosion.
- Hormonal changes (e.g., estrogen drop) amplify immune‑bone interactions, raising osteoporosis risk.
- Targeting inflammation through diet, movement, and adequate vitamin D can slow bone loss.
- Talking to your doctor about inflammatory markers is as important as checking bone density.
What Is Bone Loss?
Bone loss is a gradual reduction in bone mass and structural integrity, often measured by a decrease in bone mineral density (BMD). When loss becomes severe, it leads to osteoporosisa condition characterized by porous, fragile bones that break easily. The process begins at the microscopic level: cells called osteoclasts resorb bone faster than osteoblasts can rebuild it.
How the Immune System Talks to Bone
The immune systema network of cells, tissues, and signaling molecules that defends the body against pathogens isn’t limited to fighting germs. It constantly monitors tissue health, and when it senses danger, it releases cytokines-tiny proteins that act as messengers. Some of those cytokines double‑check the work of bone‑remodeling cells.

Cells on the Frontline: Osteoclasts vs. Osteoblasts
Osteoclastslarge, multinucleated cells that break down bone tissue are the demolition crew. They attach to bone surfaces, dissolve mineral matrix, and create tiny pits called resorption lacunae. In contrast, osteoblastsbone‑forming cells that lay down fresh collagen and mineral are the builders. A healthy skeleton relies on a tight balance between the two.
Immune signals can tip this balance. When pro‑inflammatory cytokines rise, they stimulate osteoclast precursors and suppress osteoblast activity, leading to net bone loss.
Cytokines: The Messengers Linking Inflammation and Bone
The most notorious player is RANKLa cytokine that binds to the RANK receptor on osteoclast precursors, driving their maturation. RANKL is produced by activated T‑cells and stromal cells during immune responses. Its natural inhibitor, osteoprotegerin (OPG), acts like a decoy, binding RANKL and preventing it from reaching RANK.
Other cytokines that promote bone loss include:
- TNF‑α - spikes during infections and autoimmune flare‑ups; it boosts RANKL expression and directly encourages osteoclast formation.
- IL‑6 - rises with chronic inflammation; it partners with RANKL to accelerate bone resorption.
- IL‑1β - another strong osteoclast stimulator, especially in rheumatoid arthritis.
Conversely, anti‑inflammatory cytokines such as IL‑4 and IL‑10 can dampen osteoclast activity, offering a protective effect.
Key Signaling Pathways
When RANKL binds to RANK on osteoclast precursors, it triggers the NF‑κB pathway, a master regulator of immune‑driven bone resorption. NF‑κB activation leads to the expression of genes that drive cell fusion, acid production, and matrix degradation.
Other pathways intersecting with bone health include:
- JAK/STAT - mediates signals from cytokines like IL‑6; JAK inhibitors used for rheumatoid arthritis have been shown to improve BMD.
- Wnt/β‑catenin - essential for osteoblast differentiation; inflammatory cytokines can suppress Wnt signaling, hampering bone formation.
Risk Factors That Combine Inflammation and Bone Loss
Several everyday factors create a perfect storm for bone loss by stoking inflammation:
- Age‑related estrogen decline: Estrogen normally helps keep RANKL in check; its loss after menopause removes this brake, leading to higher osteoclast activity.
- Obesity: Excess fat releases IL‑6 and TNF‑α, chronic low‑grade inflammation that can erode bone.
- Chronic infections or autoimmune diseases (e.g., rheumatoid arthritis, lupus): Persistent immune activation spikes bone‑resorbing cytokines.
- Vitamin D deficiency: Vitamin D modulates immune responses and supports calcium absorption; low levels aggravate both inflammation and bone loss.
- Sedentary lifestyle: Lack of mechanical loading reduces osteoblast stimulus while allowing inflammatory mediators to dominate.

Practical Strategies to Protect Bone While Calming the Immune System
Here’s a checklist you can start using today. Each item targets either inflammation, bone remodeling, or both.
- Get enough vitamin D - aim for 800-1000 IU daily if you live in a low‑sunlight region like Wellington. This helps keep the immune system in balance and improves calcium absorption.
- Eat anti‑inflammatory foods - fatty fish (rich in EPA/DHA), leafy greens, berries, and nuts supply omega‑3s and antioxidants that curb cytokine storms.
- Limit processed sugars and refined carbs - they trigger spikes in IL‑6 and TNF‑α.
- Maintain weight‑bearing exercise - brisk walking, jogging, or resistance training stimulates osteoblasts and lowers systemic inflammation.
- Prioritize sleep - 7-9 hours supports hormone regulation (including growth hormone and cortisol) that influences bone turnover.
- Consider targeted supplements - calcium (1,000mg/day) with magnesium, and if needed, a low‑dose bisphosphonate prescribed by a clinician for high‑risk patients.
- Screen inflammatory markers - discuss CRP, ESR, and RANKL/OPG ratios with your doctor, especially if you have a chronic condition.
Comparison of Pro‑Bone vs. Pro‑Bone‑Loss Cytokines
| Category | Cytokine | Primary Effect on Bone |
|---|---|---|
| Pro‑Bone (protective) | IL‑4 | Inhibits osteoclast formation, promotes osteoblast activity |
| Pro‑Bone (protective) | IL‑10 | Suppresses inflammatory signaling, reduces RANKL expression |
| Pro‑Bone‑Loss | RANKL | Drives osteoclast differentiation and activation |
| Pro‑Bone‑Loss | TNF‑α | Enhances RANKL production, directly stimulates osteoclasts |
| Pro‑Bone‑Loss | IL‑6 | Synergizes with RANKL, promotes osteoclast survival |
| Pro‑Bone‑Loss | IL‑1β | Accelerates bone resorption, up‑regulates RANKL |
Frequently Asked Questions
Can an infection really cause my bones to become weaker?
Yes. Acute infections lift levels of cytokines such as TNF‑α and IL‑6, which signal osteoclasts to increase bone resorption. In most healthy adults the effect is temporary, but repeated infections or chronic inflammation can lead to measurable loss in bone density.
Is osteoporosis considered an immune‑mediated disease?
Osteoporosis itself is a skeletal disorder, but many of its triggers-post‑menopausal estrogen loss, rheumatoid arthritis, chronic glucocorticoid use-are driven by immune mechanisms. So while not purely immune‑mediated, the disease is heavily influenced by the immune system.
Should I get my RANKL levels tested?
RANKL testing is not routine for most people. It becomes relevant if you have an autoimmune condition, are on long‑term steroids, or have unexplained rapid bone loss. Discuss with your physician to see if specialized labs are needed.
Do anti‑inflammatory drugs protect bone?
Non‑steroidal anti‑inflammatory drugs (NSAIDs) can lower cytokine spikes, but evidence for long‑term bone protection is mixed. Targeted therapies like TNF inhibitors have stronger data showing improved bone density in rheumatoid arthritis patients.
What lifestyle tweak gives the biggest bang for my bone health?
Weight‑bearing exercise combined with a diet rich in omega‑3 fatty acids and adequate vitamin D consistently ranks highest for both lowering inflammation and stimulating bone formation.
Next Steps & Troubleshooting
If you notice unexpected joint pain, frequent fractures, or a sudden dip in BMD scores, follow this quick flow:
- Schedule a bone density scan (DXA) to establish a baseline.
- Ask your doctor to order inflammatory markers (CRP, ESR, possibly RANKL/OPG).Review medication list - steroids, some anti‑depressants, and certain anticonvulsants can aggravate bone loss.
- Implement the lifestyle checklist above for at least three months, then reassess labs.
- If markers remain high, consider referral to a rheumatologist for targeted anti‑cytokine therapy.
Understanding that bone loss and immunity are two sides of the same coin empowers you to act early. By keeping inflammation in check and feeding your skeleton the nutrients it craves, you can slow the march toward fragile bones and stay active for years to come.

Write a comment