Many people with chronic pain are told to try antidepressants - not because they’re depressed, but because these drugs can actually change how the brain processes pain. Escitalopram, a common SSRI, is one of them. You might have heard it’s for anxiety or depression. But what if your back hurts every day, or your nerves burn from old injuries? Could escitalopram help with that too?
How Escitalopram Works Beyond Mood
Escitalopram is sold under brand names like Lexapro and Cipralex. It’s an SSRI - selective serotonin reuptake inhibitor. That means it keeps more serotonin floating around in your brain. Serotonin isn’t just a ‘happiness chemical.’ It’s deeply involved in how your nervous system handles pain signals.
Chronic pain often isn’t just from damaged tissue. It’s from your nerves becoming hypersensitive. Think of it like a faulty alarm system that goes off even when there’s no fire. Escitalopram helps calm that overactive signal. Studies show SSRIs like escitalopram can reduce pain intensity in conditions like fibromyalgia, diabetic neuropathy, and chronic lower back pain - even when depression isn’t present.
A 2023 meta-analysis in The Journal of Pain reviewed 17 randomized trials involving over 1,800 patients. Those taking escitalopram reported a 30% average reduction in pain scores compared to placebo. That’s not a cure, but for someone who’s been stuck at an 8/10 pain level for years, dropping to 5 or 6 can mean the difference between staying in bed and walking the dog.
Which Types of Chronic Pain Respond Best?
Not all chronic pain is the same. Escitalopram works best when the pain has a strong nerve component - what doctors call neuropathic or centralized pain.
- Diabetic neuropathy: Burning, tingling feet or hands. Escitalopram helps reduce those sharp, shooting pains better than many traditional painkillers.
- Fibromyalgia: Widespread muscle pain, fatigue, sleep issues. SSRIs like escitalopram are often part of first-line treatment guidelines in Europe and Canada.
- Chronic tension headaches and migraines: While not as strong as tricyclics, escitalopram can reduce frequency and severity over time.
- Post-surgical or post-injury pain: Especially when pain lingers past healing time, escitalopram may help reset nerve sensitivity.
It doesn’t work as well for mechanical pain - like a bad hip from arthritis or a herniated disc pressing on a nerve. Those usually need physical therapy, injections, or other targeted treatments.
How Long Does It Take to Work for Pain?
If you’re expecting quick relief, you’ll be disappointed. Escitalopram doesn’t act like ibuprofen. It takes weeks - sometimes up to eight - to show noticeable pain reduction.
Most people start feeling small changes around week 3: maybe the burning in their feet isn’t as sharp, or they can sit through a movie without needing to shift positions. Full benefit often hits between weeks 6 and 10. That’s why doctors usually give it a full 12-week trial before deciding if it’s working.
And here’s the catch: if you stop taking it too early, you might never know if it could’ve helped. Many patients quit at week 4 because they didn’t feel better yet - and miss out on real improvement.
Dosage and How It’s Used for Pain
For depression, the usual starting dose is 10 mg daily. For chronic pain, that’s often enough - and sometimes even too much.
Many pain specialists start patients at 5 mg daily, especially older adults or those sensitive to side effects. Some studies used up to 20 mg, but higher doses don’t always mean better pain control - and they increase side effects like nausea, dizziness, or sexual dysfunction.
It’s taken once a day, same time every day. Doesn’t matter if it’s morning or night - just be consistent. Some people feel slightly sleepy at first, so taking it at night helps. Others feel more alert, so morning works better. Track how you feel and adjust timing with your doctor.
Side Effects You Should Know
Escitalopram is generally well-tolerated, but it’s not harmless. Common side effects include:
- Nausea (usually fades after 1-2 weeks)
- Headaches or dizziness
- Insomnia or drowsiness
- Reduced sex drive or delayed orgasm
- Weight gain (slight, but possible over months)
Less common but serious risks include serotonin syndrome - especially if you’re taking other drugs that raise serotonin (like tramadol, certain migraine meds, or St. John’s wort). Symptoms: high fever, fast heartbeat, confusion, muscle rigidity. Seek help immediately if you notice these.
It can also worsen anxiety at first. That’s why doctors often start low and go slow. If you feel worse emotionally in the first two weeks, don’t panic - but do call your doctor. You’re not broken. Your brain is just adjusting.
Who Should Avoid It?
Escitalopram isn’t for everyone. Avoid it if you:
- Have a history of QT prolongation or heart rhythm issues
- Are taking MAO inhibitors (like phenelzine) - wait at least 14 days after stopping one before starting escitalopram
- Are under 18 - safety and effectiveness aren’t well-established in teens for pain
- Are pregnant or breastfeeding - it crosses the placenta and breast milk. Talk to your OB-GYN about risks vs. benefits
If you’ve had bad reactions to other SSRIs (like fluoxetine or sertraline), escitalopram might not be your best bet. They’re similar, and cross-reactivity is common.
How It Compares to Other Pain Meds
Here’s how escitalopram stacks up against other common options:
| Treatment | Works for Nerve Pain? | Time to Effect | Common Side Effects | Addictive? |
|---|---|---|---|---|
| Escitalopram | Yes | 4-10 weeks | Nausea, drowsiness, sexual side effects | No |
| Gabapentin | Yes | 1-4 weeks | Dizziness, weight gain, brain fog | No |
| Amitriptyline (TCA) | Yes | 2-6 weeks | Dry mouth, constipation, drowsiness | No |
| Tramadol | Yes | Days | Nausea, dizziness, risk of dependence | Yes |
| Ibuprofen (NSAID) | Usually No | Hours | Stomach upset, kidney risk | No |
Escitalopram is slower than gabapentin or tramadol, but it doesn’t cause brain fog or carry addiction risks. It’s often preferred for long-term use, especially if you also struggle with anxiety or sleep issues.

Real Stories: What Patients Say
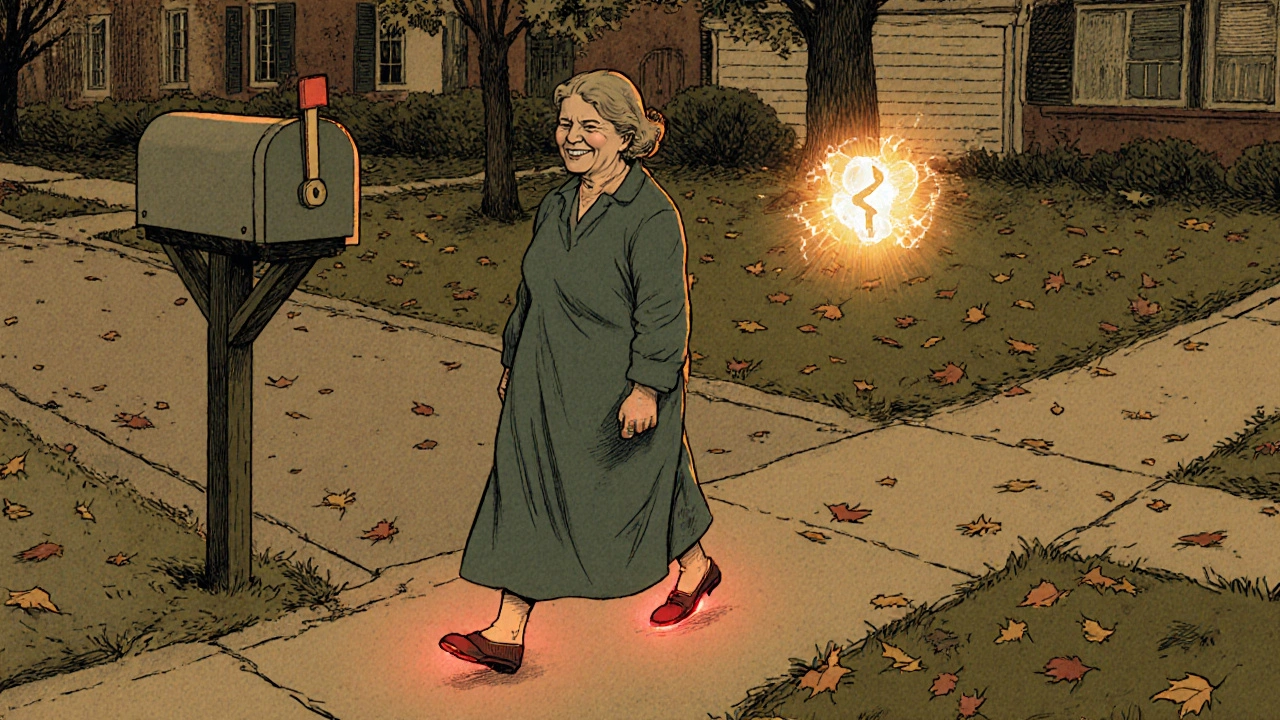
One woman in Auckland, 58, had diabetic neuropathy for 7 years. She tried gabapentin but couldn’t stand the dizziness. Her GP switched her to 10 mg escitalopram. After 8 weeks, she said: ‘I can finally walk to the mailbox without my feet feeling like they’re on fire. I still have pain, but now I can live with it.’
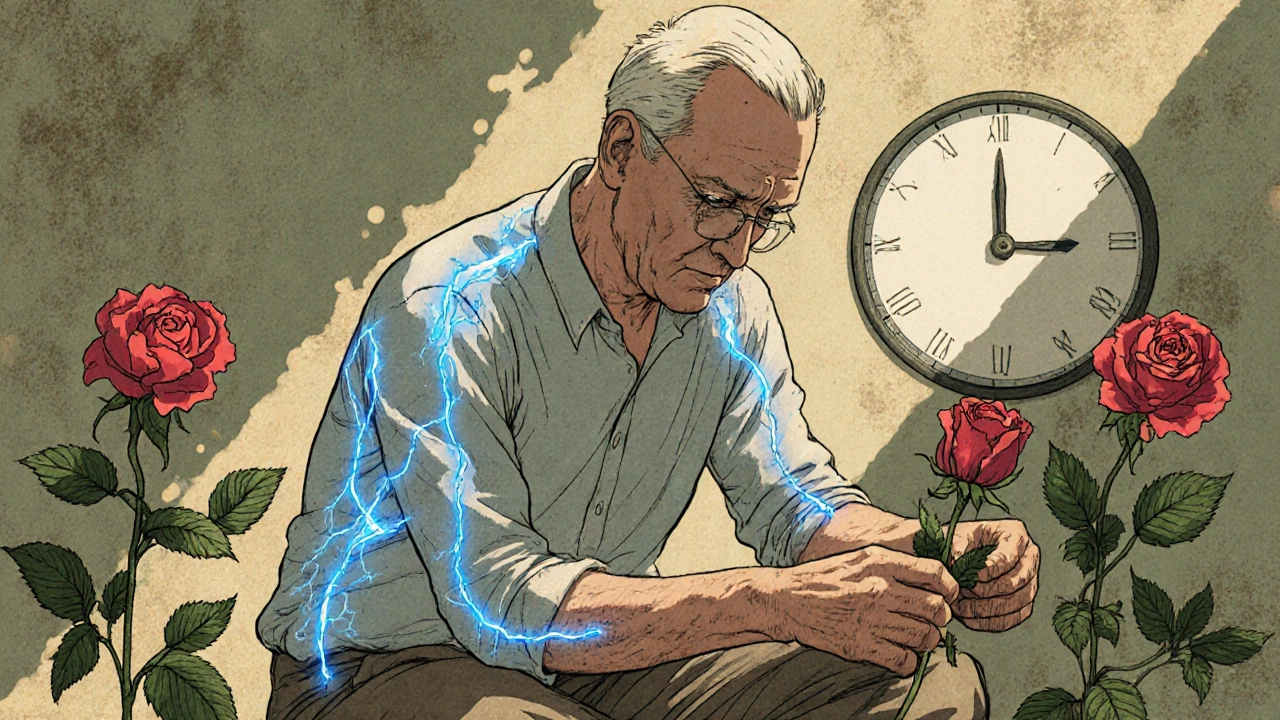
A man in Christchurch with fibromyalgia tried multiple drugs - opioids, NSAIDs, muscle relaxants. Nothing stuck. Escitalopram didn’t erase his pain, but it gave him back energy. ‘I started gardening again,’ he told his therapist. ‘That’s the first time in five years.’
These aren’t miracles. They’re improvements. And for chronic pain, improvement is often the goal.
What to Do If It Doesn’t Work
If you’ve taken escitalopram for 12 weeks at a full dose and see no change, it’s not working for you. That’s okay. Not everyone responds.
Your doctor might try:
- Switching to another SSRI (like sertraline)
- Trying a different class - SNRIs like duloxetine (Cymbalta) are often more effective for nerve pain
- Combining it with non-drug therapies: physical therapy, CBT, or mindfulness
Don’t give up on treatment just because one drug didn’t click. Chronic pain is personal. Finding the right mix takes time.
Can You Use It With Other Pain Meds?
Yes - but carefully. Escitalopram is often combined with:
- Physical therapy (highly recommended)
- Mild NSAIDs like naproxen (avoid long-term use)
- Acetaminophen (paracetamol) for occasional flare-ups
Avoid combining it with:
- Tramadol, dextromethorphan, or certain migraine meds (risk of serotonin syndrome)
- St. John’s wort, tryptophan, or 5-HTP supplements
- Alcohol - it can worsen drowsiness and depression
Always tell your doctor and pharmacist about everything you’re taking - even herbal teas or over-the-counter sleep aids.
Final Thoughts: Is It Worth Trying?
Escitalopram won’t fix every kind of chronic pain. But if your pain is rooted in nerves, not just joints or muscles, it’s one of the safest, non-addictive options available. It doesn’t just mask pain - it helps rewire how your brain perceives it.
It’s not a magic pill. It takes patience. It has side effects. But for many, it’s the first thing that actually lets them get back into life.
If you’ve been told ‘it’s all in your head’ - that’s not true. But your head does play a big role in how pain feels. Escitalopram helps fix that.
Can escitalopram cure chronic pain?
No, escitalopram doesn’t cure chronic pain. It helps reduce the intensity and impact of pain signals in the brain. For many, it turns debilitating pain into something manageable - but it doesn’t reverse the underlying damage or condition.
How long should I take escitalopram for pain?
Most doctors recommend a trial of 12 weeks to see if it works. If it helps, many people stay on it for months or years. Chronic pain often needs ongoing management, and escitalopram is safe for long-term use under medical supervision.
Will escitalopram make me feel emotionally numb?
Some people report feeling emotionally flat at first, but this usually fades. Unlike older antidepressants, escitalopram is less likely to cause emotional blunting. If you feel detached or unmotivated after several weeks, talk to your doctor - your dose may need adjusting.
Is escitalopram better than gabapentin for nerve pain?
It depends. Gabapentin works faster and is often more effective for sharp, shooting nerve pain. Escitalopram works slower but has fewer cognitive side effects like brain fog and dizziness. It’s often preferred for people who need to stay alert, or who also have anxiety or depression.
Can I stop escitalopram if my pain improves?
Don’t stop suddenly. Even if your pain is gone, your brain may still rely on the drug’s effect. Tapering off slowly over 2-4 weeks prevents withdrawal symptoms like dizziness, electric-shock sensations, or mood swings. Always work with your doctor to come off safely.

Write a comment