For years, people with chronic insomnia were told to just sleep hygiene-no caffeine after noon, keep your room dark, avoid screens before bed. It sounds simple. But if you’ve been lying awake for months, even years, you know: that advice doesn’t fix anything. You follow all the rules. You’re exhausted. You’re anxious. You’re still wide awake at 2 a.m., counting sheep that won’t come. And the next day? You’re a ghost. That’s because sleep hygiene isn’t a cure. It’s a bandage. And chronic insomnia needs surgery, not a plaster.
What Chronic Insomnia Really Means
Chronic insomnia isn’t just bad nights. It’s not stress, jet lag, or too much coffee. The American Academy of Sleep Medicine defines it clearly: trouble falling asleep, staying asleep, or waking up feeling unrefreshed-happening at least three nights a week for three months or longer. That’s not bad luck. That’s a brain that’s learned to associate your bed with wakefulness, worry, and frustration. And once that pattern sticks, no amount of lavender oil or white noise will break it.
Most people with chronic insomnia don’t sleep less than everyone else. They just think they do. Their sleep diaries show they’re getting six hours. But their brain is stuck in a loop: “If I don’t sleep eight hours, I’ll collapse at work.” That thought? It’s the real enemy. Not the darkness. Not the noise. Not even the caffeine you had at 3 p.m.
Why Sleep Hygiene Doesn’t Work for Chronic Insomnia
Sleep hygiene sounds like common sense. And it is-for people who have occasional trouble sleeping. But for those with chronic insomnia, it’s like telling someone with a broken leg to walk more carefully. It doesn’t heal the fracture.
Studies show sleep hygiene alone improves sleep by maybe 10-15%. That’s barely noticeable. The American Academy of Sleep Medicine gives it only moderate evidence. Meanwhile, the same group gives CBT-I a strong recommendation based on high-quality evidence. Why? Because CBT-I doesn’t just change habits. It rewires thoughts.
Dr. Jack D. Edinger, one of the leading researchers in this field, says flat out: “Sleep hygiene education alone is minimally effective for chronic insomnia and should not be offered as standalone treatment.” The military’s own patient guide echoes this: “Do not use sleep hygiene as a standalone treatment for chronic insomnia.” If your doctor only gave you a list of tips and called it a day, you were given incomplete care.
What CBT-I Actually Is (And Isn’t)
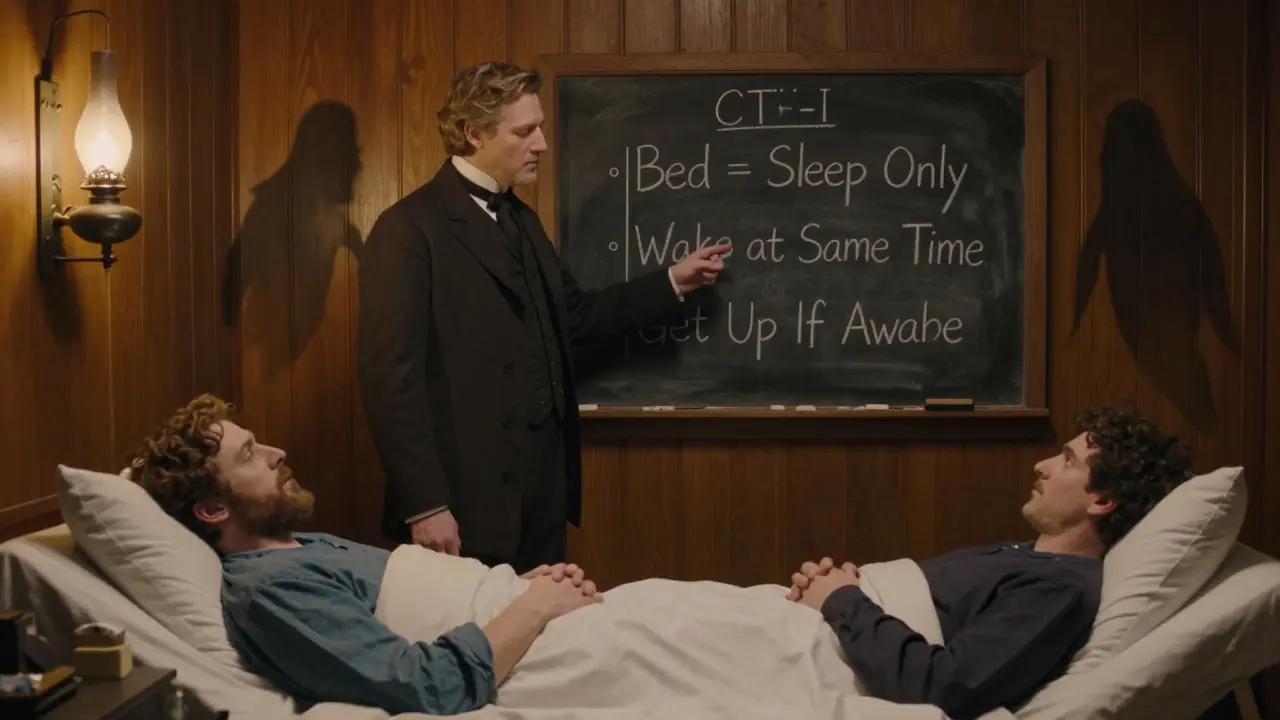
Cognitive Behavioral Therapy for Insomnia-CBT-I-isn’t therapy in the “talk about your childhood” sense. It’s a structured, time-limited program, usually six to eight weeks long, that teaches you how to break the cycle of insomnia using proven behavioral and cognitive tools. It’s not magic. It’s mechanics.
There are five core parts:
- Stimulus Control: Your bed is for sleep and sex only. No reading, no scrolling, no worrying. If you’re not asleep in 15-20 minutes, get up. Go sit in another room. Do something quiet until you feel sleepy. Then go back to bed. Repeat. This retrains your brain: bed = sleep, not stress.
- Sleep Restriction: This sounds cruel. You’re told to spend less time in bed than you think you’re sleeping. If you’re only sleeping 5 hours a night, you’re told to only be in bed 5 hours. You might feel awful for the first week. But this builds up sleep pressure. Your body starts to crave sleep. After a few weeks, you slowly add back 15 minutes of time in bed-until you find the sweet spot where you sleep well and wake up refreshed.
- Cognitive Restructuring: This is where you tackle the lies your brain tells you. “I need 8 hours.” “If I don’t sleep, I’ll lose my job.” “I’m broken.” These thoughts fuel anxiety, and anxiety kills sleep. CBT-I helps you replace them with facts: “I can function on 6 hours.” “My body adapts.” “Sleep will come when I stop fighting it.” A 2019 study found this alone reduced sleep anxiety in 65% of patients.
- Relaxation Training: Not just deep breathing. It’s progressive muscle relaxation, diaphragmatic breathing, mindfulness-tools to calm your nervous system before bed. Your body can’t be tense and asleep at the same time.
- Sleep Hygiene: Yes, it’s still part of it. But now it’s not the star. It’s the supporting actor. You do it, but only after the real work-behavioral change-is underway.
How Effective Is CBT-I?
It works. Like, really works.
Between 70% and 80% of people who complete CBT-I see clinically meaningful improvement. That means falling asleep faster, waking up less, and feeling less exhausted during the day. A 2020 meta-analysis showed CBT-I cuts sleep onset latency (how long it takes to fall asleep) by 18.2 minutes on average-and wake after sleep onset (how long you’re awake during the night) by 27.4 minutes. Compare that to sleeping pills: they reduce those numbers by 12.1 and 15.8 minutes. And here’s the kicker: the pill effects vanish the moment you stop taking them. CBT-I’s effects last. For years.
One Reddit user wrote: “After 8 weeks of CBT-I, my sleep efficiency jumped from 68% to 89%. I fall asleep in 15 minutes now instead of two hours.” Another said: “The first two weeks of sleep restriction were brutal. I felt like I was going to die. But then… it clicked.”
Even digital CBT-I programs like Sleepio and SHUTi have shown 50-60% remission rates-meaning people stop meeting the clinical definition of insomnia. That’s better than most medications. And they’re accessible. No waiting months for a therapist.
The Catch: It’s Hard at First
CBT-I isn’t easy. It’s not supposed to be. You’re asking your brain to unlearn a habit it’s had for years. That’s uncomfortable.
Sleep restriction makes you tired. Really tired. Some people quit because they can’t handle the first week. Others get stuck on stimulus control-staying in bed too long, convinced they’ll fall asleep “any minute now.”
And then there’s the access problem. In the U.S., there are only 0.5 certified CBT-I therapists per 100,000 people. In rural areas, 78% of counties have no sleep specialist at all. Insurance often covers only 3 of the 6-8 sessions you need. One user on Reddit said: “My insurance only paid for three sessions. I couldn’t finish. I gave up.”
That’s why digital options matter. Apps like Somryst are FDA-cleared as prescription digital therapeutics. They guide you through the full CBT-I protocol. A 2020 FDA submission showed 55.4% remission rates. Fitbit now even uses CBT-I principles in its Sleep Profile feature, adjusting recommendations based on 30+ nights of data.

What You Can Do Today
If you’ve been struggling with insomnia for months:
- Stop relying on sleep hygiene alone. It’s not enough.
- Track your sleep for a week. Write down when you get in bed, when you fall asleep, when you wake up, and how many times you’re awake. Use a notebook or a free app. This is your baseline.
- Set a fixed wake-up time. No exceptions. Not even on weekends. This is the most powerful single tool in CBT-I.
- If you’re not asleep after 20 minutes, get up. Go to another room. Read a boring book under dim light. Don’t check your phone. Come back only when sleepy.
- Eliminate caffeine after 2 p.m. No exceptions. Alcohol? Don’t drink it within 4 hours of bed. It might knock you out, but it shreds your deep sleep.
- Consider a digital CBT-I program. Look for ones with FDA clearance or published clinical trials. Avoid apps that just play rain sounds.
What’s Next for Insomnia Treatment?
The future is personalized. AI is starting to tailor CBT-I protocols based on your sleep patterns, stress levels, and even heart rate variability. Pear Therapeutics’ reSET-S app is in Phase 3 trials with 63% response rates at 12 weeks. Experts like Dr. Andrew Krystal predict CBT-I will become the standard for 90% of chronic insomnia cases within the next decade.
Right now, the biggest barrier isn’t science. It’s access. And cost. But the tide is turning. Thirty-seven percent of Fortune 500 companies now offer CBT-I through employee wellness programs. More insurers are starting to cover it. The digital market is projected to hit $1.2 billion by 2027.
You don’t have to live like this. Chronic insomnia isn’t your fault. It’s a learned pattern. And like any learned pattern, it can be unlearned. You don’t need a miracle. You need the right tools. And CBT-I is the only one backed by decades of science, real results, and lasting change.
Is sleep hygiene useless for chronic insomnia?
No, but it’s not enough on its own. Sleep hygiene-like keeping your room cool, dark, and quiet-helps create the right environment. But if your brain has learned to associate your bed with wakefulness and anxiety, no amount of good sleep habits will fix that. CBT-I targets the mental and behavioral patterns causing the problem. Sleep hygiene is a support tool, not the cure.
How long does CBT-I take to work?
Most people notice small improvements within 2-4 weeks, especially with consistent wake times and stimulus control. But full benefits usually take 6-8 weeks. Sleep restriction, the toughest part, often causes temporary worsening of sleep in the first week or two. That’s normal. It’s part of the process. Stick with it. The results are durable.
Can I do CBT-I without a therapist?
Yes. Several digital programs are clinically proven and FDA-cleared, like Sleepio, SHUTi, and Somryst. These apps guide you step-by-step through all five components of CBT-I. Studies show they’re just as effective as in-person therapy for most people. The key is sticking to the full program-not skipping sessions or skipping the hard parts.
Why are sleeping pills not the answer?
Sleeping pills like zolpidem or eszopiclone can help short-term, but they don’t fix the underlying problem. After 4-6 weeks, their effectiveness drops. You can develop tolerance, dependence, or side effects like dizziness or memory issues. Worse-they don’t improve daytime functioning the way CBT-I does. Once you stop taking them, insomnia usually comes back. CBT-I teaches you to sleep without drugs-and keeps working long after you stop.
What’s the Insomnia Severity Index (ISI)?
The ISI is a 7-question questionnaire doctors and researchers use to measure how bad your insomnia is. Scores from 0-7 mean no insomnia, 8-14 is mild, 15-21 is moderate, and 22-28 is severe. If your score is above 15, you likely need more than sleep hygiene. CBT-I is the recommended next step. Many digital programs include the ISI to track your progress.
Is CBT-I worth it if I’m older?
Absolutely. Studies show CBT-I works just as well in older adults as it does in younger people. In fact, it’s often preferred over medication for seniors because it avoids the risks of drowsiness, falls, and confusion. The American Academy of Sleep Medicine recommends CBT-I for all adults, including those over 65. Sleep changes with age-but insomnia doesn’t have to be inevitable.
If you’ve tried everything and still can’t sleep, it’s not you. It’s the treatment. CBT-I isn’t just another tip. It’s the only treatment proven to change the brain’s relationship with sleep-for good.


Write a comment