When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But behind that simple promise is a complex, tightly controlled environment - a cleanroom - where every particle, breath, and movement is monitored to protect drug quality. For generic drug makers, meeting these standards isn’t optional. It’s the difference between a life-saving medication and a dangerous failure.
Why Cleanrooms Matter More for Generic Drugs
Generic drugs aren’t copies. They’re required to be bioequivalent - meaning they deliver the same amount of active ingredient at the same rate as the original drug. But here’s the catch: if the generic is contaminated, even slightly, it can change how the drug behaves in your body. A single particle of mold or a stray fiber from a technician’s suit can alter dissolution rates or introduce harmful microbes. That’s why cleanroom standards exist.The FDA and other global regulators don’t treat generic manufacturers any differently than innovators. If a brand-name injectable is made in a Grade A cleanroom, so must the generic. There’s no lower bar. In fact, generic companies often face more scrutiny because they’re under pressure to cut costs - and that makes compliance harder.
The Four Levels of Cleanroom Grades
Pharmaceutical cleanrooms are divided into four grades, each with strict limits on particles and microbes. These aren’t arbitrary numbers - they’re based on decades of science and real-world contamination events.- Grade A (ISO Class 5): The highest level. Used for filling sterile products like injectables. No more than 3,520 particles larger than 0.5 micrometers per cubic meter. Air flows in a single direction, like a silent waterfall, sweeping contaminants away. Temperature? 18-26°C. Humidity? 30-60%. One mistake here can trigger a recall.
- Grade B (ISO Class 5 at rest, ISO Class 7 operational): The background environment for Grade A. Think of it as the control room. Particle counts jump during operations, but continuous monitoring catches spikes before they become problems.
- Grade C (ISO Class 7 at rest, ISO Class 8 operational): Where you prepare solutions and sterilize equipment. Particle limits are higher, but still tight enough to prevent cross-contamination.
- Grade D (ISO Class 8 at rest): The lowest level, used for packaging or less sensitive steps. Still requires 10 air changes per hour and strict gowning.
These grades aren’t just European or American rules. ISO 14644-1, the global standard, is used everywhere from India to Brazil. Even if your country doesn’t enforce it directly, the FDA will inspect your facility - and if it doesn’t meet ISO Class 5 for sterile products, your drugs won’t be allowed into the U.S. market.
What Happens When Standards Are Broken
In 2012, the New England Compounding Center’s dirty steroid injections killed 64 people and sickened over 750. The root cause? No cleanroom. No filtration. No monitoring. It wasn’t a technical glitch - it was negligence.Today, the consequences are just as severe, even if less deadly. In 2022, the FDA issued 228 warning letters for cGMP violations - 63% of all warning letters that year. Aurobindo Pharma paid $137 million in recalls after failing to monitor Grade B air quality properly. Teva had to delay approval of a generic cancer drug because particle counts spiked during technician movement.
These aren’t rare. The FDA’s 2022 report showed 42% of complete response letters for sterile generics cited environmental monitoring failures - up from 31% in 2018. That means more rejections, longer delays, and lost revenue.
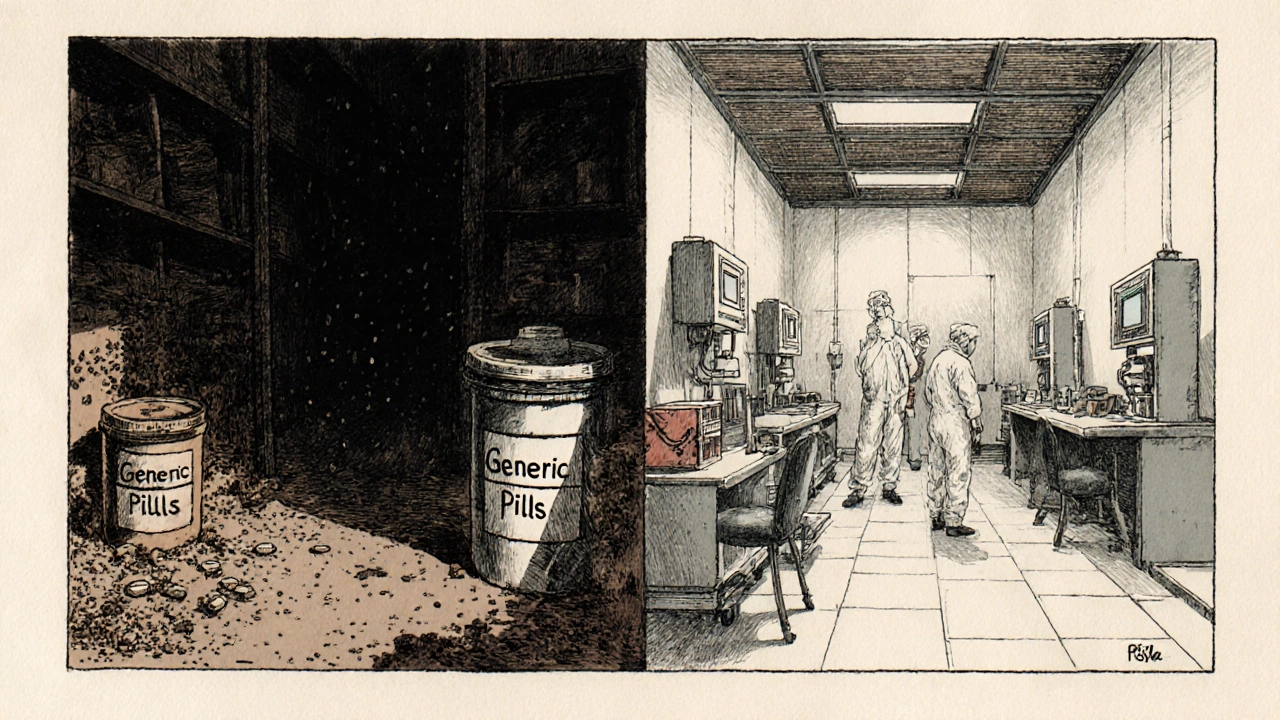
Costs That Break Small Manufacturers
Building a Grade A cleanroom costs between $250 and $500 per square foot. For a small facility making a $0.50-per-unit generic heparin syringe, that’s a death sentence. One Reddit user from a small generic company said: “We spent $3 million upgrading our cleanroom. After the third FDA inspection, we were still getting particle excursions. We couldn’t afford to keep going.”Big companies like Pfizer can absorb $2.3 million HVAC upgrades. But for many generic manufacturers, cleanroom compliance eats up 15-25% of total capital spending - compared to 10-15% for brand-name firms. That’s why many outsource sterile production to specialized contract manufacturers, even if it cuts into margins.
And it’s not just construction. Training staff to gown properly takes 40-60 hours. Validation alone - proving the room works as designed - costs $150,000 to $500,000 and takes 3-6 months. Then there’s the ongoing cost: continuous particle monitors, HEPA filter replacements, microbial sampling, and documentation for 15-20 SOPs.
Where Standards Are Too Much - And Where They’re Not Enough
Not everyone agrees that every drug needs a Grade C cleanroom. Dr. Paul K. S. Shin argues that for oral solids - pills and capsules - Grade D should be enough. A 2020 study showed identical dissolution profiles between Grade D and Grade C facilities. Why spend extra if the drug works the same?But for sterile products? No debate. Injectables, eye drops, and inhalers can’t afford contamination. The FDA’s 2023 Strategic Plan says 50% of new generic applications by 2025 will need Grade A/B environments - up from 35% in 2022. Why? Because more generics are now complex: biologics, biosimilars, and combination products. These aren’t simple pills. They’re living systems that demand extreme control.
And then there’s the problem of tropical climates. In India or Southeast Asia, humidity can hit 90%. Standard HVAC systems can’t keep moisture under 60% without adding 20-30% to energy costs. Some manufacturers install desiccant dehumidifiers - expensive, noisy, and power-hungry - just to meet the numbers.
How the Best Manufacturers Succeed
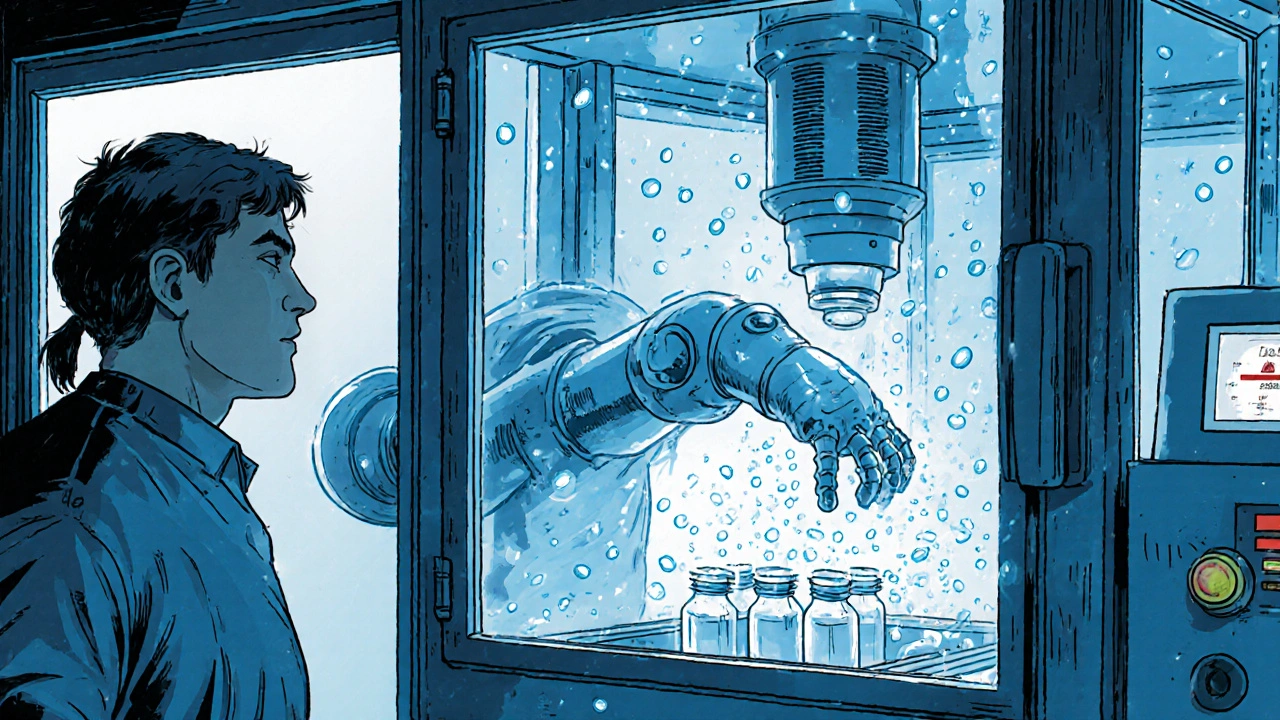
Success isn’t about spending the most. It’s about controlling what matters.Teva’s generic version of Copaxone used advanced isolators - sealed, robotic systems that keep humans out of the critical zone. Contamination events dropped from 12 per year to just 2. That’s how they got FDA approval after two prior rejections.
Others use real-time monitoring. Instead of waiting for weekly air samples, sensors track particles every second. If a technician opens a door and the count spikes, the system alerts supervisors before a batch is made. These systems cost $50,000-$100,000 per room - but they prevent millions in losses.
Automation is the future. Robots now load vials, seal containers, and even clean surfaces. One McKinsey study predicts automation will cut cleanroom operational costs by 25-30% by 2028. That could be the lifeline small generic makers need.
What You Need to Know as a Patient
You don’t need to understand ISO classifications or HEPA filters. But you should know this: when you take a generic drug, you’re trusting a system designed to prevent harm. Every cleanroom standard exists because someone once got sick - or died - from a contaminated pill.The FDA doesn’t approve a generic unless it’s proven safe, effective, and made under the same quality controls as the brand. That’s why you can trust a generic. But it’s not magic. It’s science. It’s hours of training. It’s machines running 24/7. It’s people in bunny suits, moving slowly, breathing carefully.
When you see a generic on your receipt, remember: behind that low price is a high-stakes battle against invisible threats. And the cleanroom is the frontline.
What’s Changing in 2025
The EU’s revised Annex 1 (effective August 2023) is now the global benchmark. It demands continuous monitoring, better risk assessments, and tighter control of personnel behavior. The FDA is catching up - new guidance is expected in early 2025.Also emerging: single-use systems. Instead of cleaning stainless steel tanks, manufacturers use disposable bags and tubing. Less cleaning means less contamination risk. The Parenteral Drug Association is finalizing Technical Report 81 on this, expected in 2024.
And don’t forget GDUFA III - the FDA’s 2023-2027 plan that allocates $15 million just to train inspectors on cleanroom compliance. That’s a signal: they’re watching closer than ever.
What is the difference between Grade A and Grade B cleanrooms?
Grade A is the highest level, used for direct product filling (like injecting medicine into vials). It must have no more than 3,520 particles ≥0.5μm per cubic meter, with unidirectional airflow and continuous monitoring. Grade B is the surrounding environment - it supports Grade A. At rest, it matches Grade A limits, but during operations, it allows up to 3.5 million particles. It’s not sterile on its own, but it keeps contaminants from reaching Grade A.
Do all generic drugs need a cleanroom?
Yes - but the level depends on the drug. Oral tablets and capsules need at least Grade D. Injectable drugs, eye drops, and inhalers require Grade A or B. Even non-sterile products need controlled environments to prevent cross-contamination from other drugs or foreign particles. The FDA doesn’t allow manufacturing in open warehouses or uncontrolled spaces.
How often are cleanrooms inspected?
FDA inspections for generic drug facilities happen every 2-3 years on average, but high-risk sites - like those making sterile products - can be inspected more often. If a company has prior violations, inspections may be unannounced. The EU and other regulators follow similar schedules. Cleanrooms are also monitored daily through automated systems and weekly through manual swab and air sampling.
Can a cleanroom ever be 100% contamination-free?
No. Even the best cleanrooms have some particles. The goal isn’t perfection - it’s control. Standards set limits that ensure contaminants stay below levels that could affect drug safety or performance. That’s why monitoring is continuous and why procedures like gowning and airflow management are so strict. It’s about risk reduction, not elimination.
Why do cleanroom costs vary so much between countries?
Infrastructure differences drive the cost gap. In the U.S. and EU, power, water, and HVAC systems are already advanced, so upgrades are easier. In countries like India or Nigeria, facilities often need to rebuild entire electrical and climate systems just to meet basic humidity and temperature controls. That adds $1-$1.5 million to the cost. Labor training and regulatory experience also play a role - places with less experience in GMP face steeper learning curves.


Write a comment