Every year, Americans fill over 3.9 billion prescriptions. Nearly 90% of those are for generic drugs. Yet, those same generics cost just 12% of what brand-name drugs do. That’s not a coincidence. It’s the result of a system that works - if it’s allowed to.
How Much Are You Really Saving?
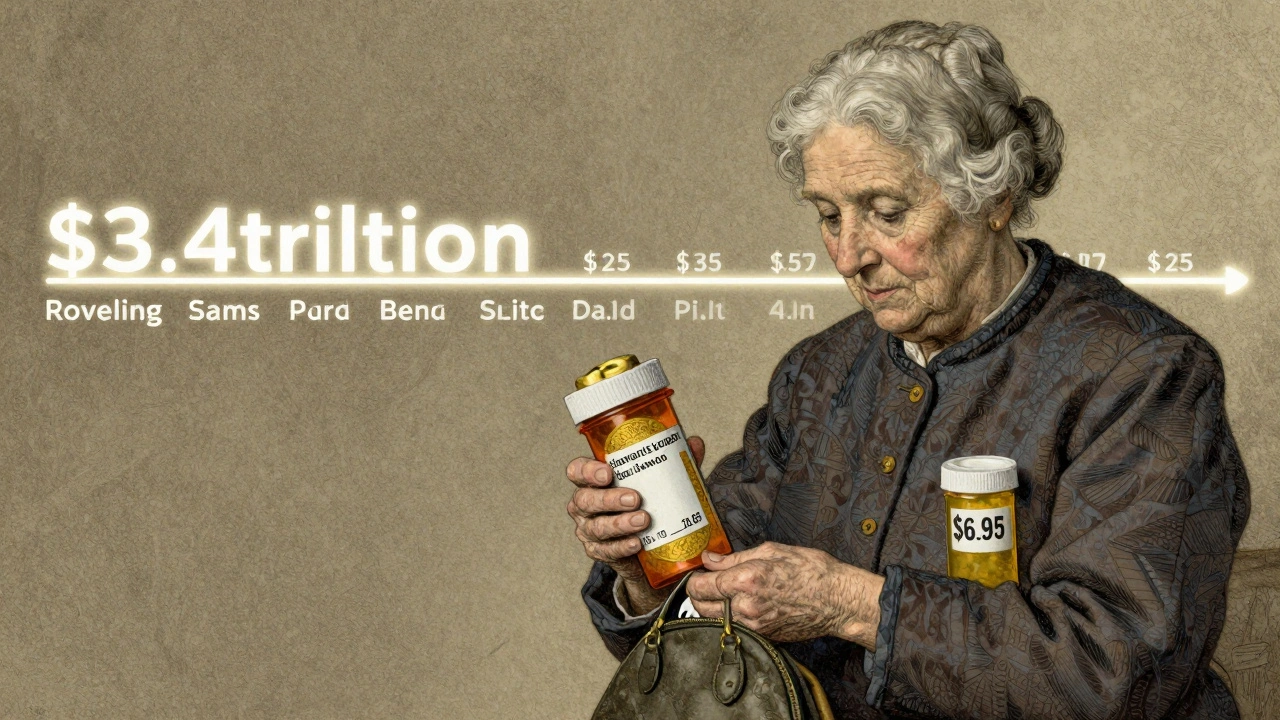
In 2024, generic and biosimilar drugs saved the U.S. healthcare system $467 billion. That’s not a guess. That’s the official number from the Association for Accessible Medicines and The IQVIA Institute. Over the past decade, that adds up to more than $3.4 trillion in savings. For most people, that means paying $6.95 for a month’s supply of a generic medication - compared to $28.69 for the brand-name version. For someone without insurance, the gap is even wider: brand-name drugs cost over $130 per prescription, while generics dropped to $6.95, down from $9.40 just five years ago.That’s a five-fold difference. If you take five prescriptions a month, you’re saving over $100 a month just by choosing generics. That’s $1,200 a year. For seniors on fixed incomes, that’s groceries, gas, or rent. For families, it’s keeping the lights on.
Why Do Generics Cost So Much Less?
Generics aren’t cheaper because they’re lower quality. They’re cheaper because they don’t have to repeat the billion-dollar clinical trials that brand-name companies do. Once a patent expires, other manufacturers can produce the same active ingredient. The FDA requires them to prove they’re bioequivalent - meaning they work the same way in your body. That’s it. No marketing budgets. No celebrity ads. No patent extensions.Since 2019, the total amount spent on all generic drugs in the U.S. has actually gone down by $6.4 billion - even though more people are using them. Prescription volume for oral generics (pills and capsules) rose from 167 billion units in 2015 to 197 billion in 2024. That’s a 15% increase in usage. But spending? Down. That’s the definition of deflation. And it’s happening in a market where brand-name drug prices keep rising.
Biosimilars: The New Frontier of Savings
Biosimilars are the next wave. They’re not exact copies like generics - they’re highly similar versions of complex biologic drugs used for cancer, arthritis, and autoimmune diseases. They’re harder to make, but they’re still cheaper. In 2024, biosimilars saved $20.2 billion - nearly double what they saved the year before. Since their launch in 2015, they’ve saved $56.2 billion total. And over 60% of those savings came in just the last two years.These drugs have been used in nearly 3.3 billion days of patient therapy with no new safety concerns. That’s not a small number. That’s millions of people getting life-saving treatment at a fraction of the cost. A single brand-name biologic can cost $20,000 a year. A biosimilar? Often under $5,000.
The Brand-Name Price Problem
While generics keep getting cheaper, brand-name drug makers keep raising prices. In January 2025, the biggest pharmaceutical companies increased prices on 250 drugs by a median of 4.5%. That’s nearly double the rate of general inflation. One drug, Vasostrict, saw its list price drop 76% in just three months - but that’s rare. Most brand-name drugs don’t drop. They climb.Specialty drugs - mostly brand-name biologics - are projected to make up 60% of all drug spending by 2025. Yet they account for less than 10% of prescriptions. That’s the real cost crisis. Generics and biosimilars make up 90% of prescriptions but only 1.2% of total healthcare spending. They’re the backbone of affordability.
What’s Threatening the Savings?
Here’s the problem: the system that saves you money is under pressure. Generic manufacturers are operating on razor-thin margins. When a drug sells for $0.10 a pill, there’s no room for error. If a factory shuts down, or if a company can’t make a profit, the drug disappears. That’s not theory. It’s happened. Over 200 drugs have had shortages in the last five years, many of them generics.Why? Because pharmacy benefit managers (PBMs) and Medicare policies often block access. They push for the cheapest option - but not always the one that’s actually available. Some payers prefer brand-name drugs because they get rebates. That’s called “product hopping.” It’s legal. It’s harmful. It drives up costs.
Another issue: pay-for-delay deals. Brand-name companies pay generic makers to delay launching their cheaper versions. A 2025 study found these deals cost the system $12 billion a year - $3 billion of that borne by Medicare. Banning them could save $45 billion over 10 years.

How Medicare Benefits - And Who Pays
Medicare saved $142 billion in 2024 thanks to generic drugs. That’s $2,643 per beneficiary. That’s not just money saved. That’s fewer people skipping doses. Fewer hospital visits. Fewer complications. When a senior can afford their blood pressure pill, they’re less likely to end up in the ER.But here’s the catch: Medicare’s new price controls under the Inflation Reduction Act are designed to cap brand-name drug prices. That’s good. But if those policies don’t also protect generic manufacturers - if they make it even harder for them to stay in business - we risk losing the very drugs that keep costs down.
What You Can Do
You don’t need to wait for Congress to fix this. Start today:- Always ask your pharmacist: “Is there a generic version?”
- If your doctor prescribes a brand-name drug, ask if a generic is available - and if it’s covered by your plan.
- Use mail-order pharmacies or discount programs like GoodRx. They often list the lowest cash price for generics.
- Don’t assume your insurance will automatically pick the cheapest option. Check your formulary.
- If a generic isn’t available, ask your doctor about biosimilars for biologic drugs - especially for conditions like rheumatoid arthritis or Crohn’s disease.
Every time you choose a generic, you’re not just saving yourself money. You’re helping keep the system alive. When enough people do it, manufacturers can keep producing. When manufacturers keep producing, shortages drop. When shortages drop, prices stay low.
The Bigger Picture
The U.S. spends more on prescription drugs than any other country - often three to five times more. Yet we’re getting less for it. Generics and biosimilars are the reason we’re not spending even more. They’re the quiet heroes of the system. No ads. No lobbyists. Just science, competition, and lower prices.But that system is fragile. It needs policy changes - like ending pay-for-delay, stopping patent abuse, and fixing how PBMs operate. But it also needs you. Your choices matter. Your questions matter. Your willingness to ask for the generic? That’s what keeps the savings flowing.
Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re bioequivalent - meaning they work the same way in your body. Generic drugs undergo the same strict manufacturing standards. The only differences are in inactive ingredients, like fillers or dyes, which don’t affect how the drug works.
Why do some generics cost more than others?
Price differences between generics come from competition. If only one company makes a generic, it may charge more. When multiple manufacturers enter the market, prices drop. For example, the generic version of Lipitor (atorvastatin) dropped to under $10 a month after six companies started making it. But if a drug has only one or two makers, prices can stay higher. Always compare prices at different pharmacies - even within the same chain.
Can I trust generics if they look different from the brand-name drug?
Absolutely. Generic drugs are allowed to look different - different color, shape, or size - because trademark laws prevent them from looking exactly like the brand-name version. But the active ingredient, dosage, and effectiveness are identical. If you’re unsure, check the label or ask your pharmacist. The FDA database also lists approved generics with their appearance details.
Why are some drugs still expensive even when generics exist?
Some drugs are still expensive because of how insurance works. Pharmacy benefit managers (PBMs) sometimes negotiate rebates with brand-name companies, making it more profitable for insurers to cover the brand-name drug even when a cheaper generic is available. This is called “non-formulary placement.” You may need to request a prior authorization or file an appeal to get coverage for the generic. Always ask your pharmacist if your plan is steering you toward the more expensive option.
Do biosimilars work the same as biologics?
Yes. Biosimilars are not exact copies, but they are highly similar to their reference biologic drugs in structure, function, and clinical effect. They’re tested in large studies to prove they produce the same results with no clinically meaningful differences. The FDA approves them only after rigorous review. For conditions like rheumatoid arthritis, psoriasis, or cancer, biosimilars have been used safely for years with outcomes matching the original biologics.
What’s the biggest threat to generic drug savings?
The biggest threat is unsustainable pricing. Generic manufacturers operate on tiny margins - sometimes pennies per pill. When prices drop too low, companies stop making the drug. That leads to shortages. In 2024, over 200 drugs faced shortages, many of them generics. Without policy changes to protect manufacturers - like ending pay-for-delay deals and stopping patent abuse - we risk losing access to affordable medications altogether.


Write a comment