When a hospital decides to add a generic drug to its formulary, it’s not just a matter of picking the cheapest option. It’s a careful, evidence-based process that involves doctors, pharmacists, economists, and sometimes even patients. The goal? To give people the safest, most effective treatment at the lowest possible cost - without cutting corners on care.
What Exactly Is a Hospital Formulary?
A hospital formulary is a living list of approved medications. It’s not a static catalog you print once a year. It’s updated regularly - often quarterly - based on new data, drug shortages, or changes in clinical guidelines. In U.S. hospitals with 100 or more beds, 98% have a formal formulary system. These are called closed formularies, meaning only approved drugs are routinely stocked and prescribed. If a doctor wants to use something outside the list, they usually need special approval. The formulary isn’t just about what’s available. It’s about what works best in real hospital settings. For example, a generic blood pressure pill might be cheaper than another, but if it causes more dizziness in elderly patients, it won’t make the cut. The system is designed to balance clinical outcomes with financial reality.How Generic Drugs Get Approved
Before a generic drug even reaches the formulary committee, it’s already been approved by the FDA. But that’s just the starting point. The FDA’s Orange Book tells hospitals whether a generic is therapeutically equivalent to the brand-name drug - meaning it delivers the same active ingredient at the same rate and amount. That’s the legal baseline. But hospitals go further. They look at:- **Clinical evidence**: At least 15-20 peer-reviewed studies on efficacy and safety for that drug class.
- **Safety data**: Adverse event rates from the FDA’s MedWatch database and hospital internal reports.
- **Cost-effectiveness**: Not just the price per pill, but how it affects hospital stays, readmissions, and complications.
- **Formulation differences**: A generic with a different filler or coating might affect absorption in patients with kidney disease or swallowing issues.
- **Supply reliability**: One manufacturer’s generic might be cheaper, but if they’ve had three shortages in a year, it’s a risk.
Why Tiers Matter
Most hospital formularies are divided into tiers. Generic drugs almost always sit in Tier 1 - the lowest cost tier for patients. That means if a patient needs a statin or an antibiotic, the hospital pushes them toward the formulary-approved generic because it’s proven, safe, and affordable. But tiers aren’t just for billing. They’re tools for clinical control. For example, if a patient has heart failure, the formulary might list three different ACE inhibitors, but only one is preferred because it has the strongest data in that population. Pharmacists are trained to substitute automatically - unless the doctor specifically says no. This is called therapeutic interchange. It’s not a loophole. It’s a standard practice in 87% of U.S. hospitals. A pharmacist can swap a non-formulary generic for a preferred one without calling the doctor - as long as the drugs are equivalent. It saves time, reduces errors, and cuts costs.
Real-World Challenges
It sounds simple, but it’s messy in practice. One hospital in Massachusetts had to temporarily remove a generic anticoagulant from its formulary seven times in 2022 because the manufacturer ran out of supply. That meant staff had to scramble to find alternatives, train nurses on new dosing, and explain the change to patients. One nurse told an online forum: “We had two medication errors in one week because people forgot the new pill looked different.” Doctors, too, get frustrated. A 2021 survey of 1,200 U.S. physicians found 41% said formulary restrictions had delayed care - especially for rare conditions or complex cases. A cancer patient might need a generic version of a drug that’s not on the list, and getting approval can take days. And then there’s the industry pressure. Pharmaceutical reps still visit hospitals, even if they’re not allowed to influence decisions directly. A 2021 study in JAMA Internal Medicine showed that even with conflict-of-interest disclosures, detailing can subtly shift prescribing habits. That’s why top hospitals now require annual training for all P&T members on how to spot and avoid bias.What’s Changing Now?
The biggest shift in recent years is moving from acquisition cost to total cost of care. A generic drug might cost $0.10 per pill, but if it causes more side effects, leading to longer hospital stays or emergency visits, it’s not really cheaper. Hospitals are now using predictive analytics to model this. Johns Hopkins saved $1.2 million a year just by switching to preferred generic anticoagulants - not because they were cheaper, but because they reduced bleeding events and readmissions. Another trend? Pharmacogenomics. Some academic hospitals are starting to use genetic data to guide formulary choices. If a patient has a gene variant that makes them metabolize a drug slowly, the formulary might prioritize a different generic version - even if it’s slightly more expensive. It’s personalized medicine, built into the system. The Inflation Reduction Act of 2022 is also pushing hospitals to align with Medicare’s new drug pricing rules. By 2025, many formularies will need to reflect those caps. And by 2028, the Agency for Healthcare Research and Quality predicts all Medicare-certified facilities will be required to have a formal formulary system.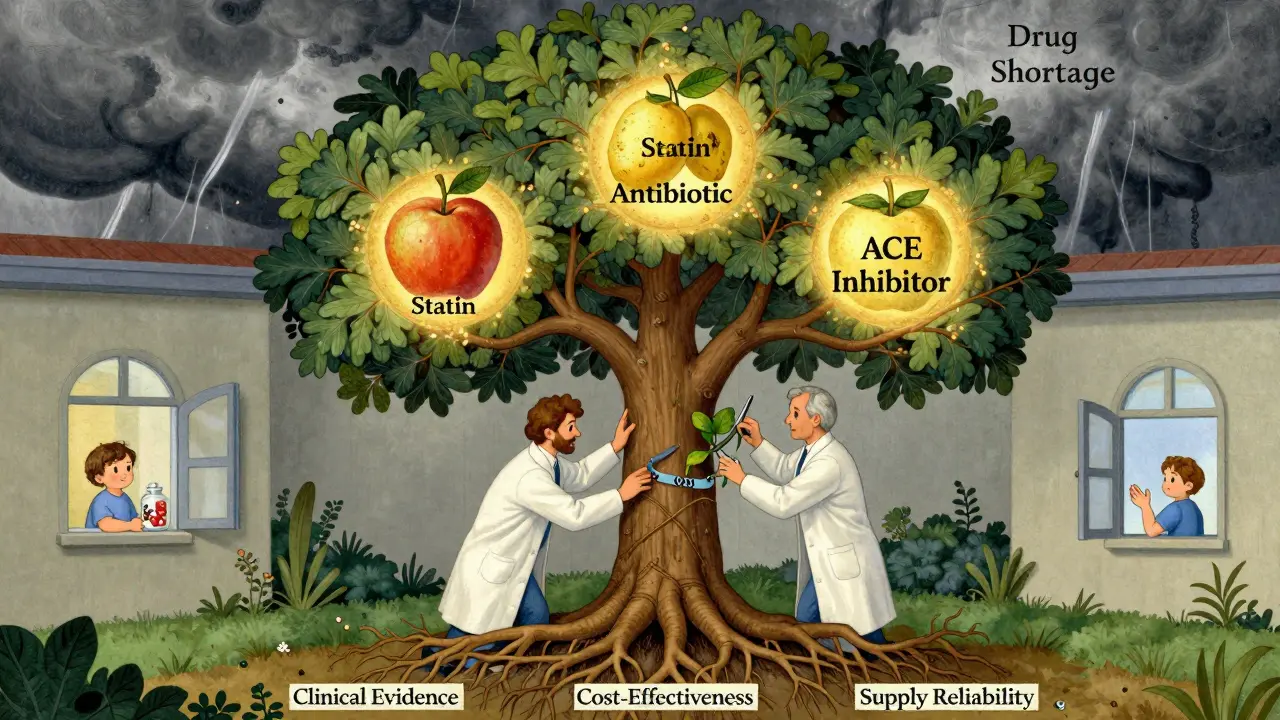
Who Decides?
The P&T committee is the heart of the system. It usually has 12 to 15 members: clinical pharmacists (often board-certified), hospitalists, specialists, a pharmacist specializing in infectious disease, and sometimes a hospital economist. They meet monthly. Each drug request comes with a dossier - 20+ pages of clinical studies, pharmacokinetic data, cost analyses, and manufacturer disclosures. The review takes 45 to 60 days. For urgent cases - like a new generic for a life-saving drug during a shortage - they can fast-track it in two weeks. At Mayo Clinic, they’ve created a separate “therapeutic alternatives committee” to handle shortages. When a generic disappears, they already have two or three backup options pre-vetted. That’s why their success rate in avoiding care disruptions is 98%.What About Biosimilars?
Biosimilars - the generic version of complex biologic drugs like Humira or Enbrel - are the next frontier. But they’re not simple generics. Their manufacturing is so complex that small changes can affect how they work. Right now, only 37% of hospital formularies have formal protocols for evaluating biosimilars. That’s a gap. The FDA says they’re safe, but hospitals want more real-world data before fully adopting them. Some are waiting for outcomes studies from large health systems before making the switch.Why This System Works
Despite the headaches, hospital formularies save money without sacrificing safety. Hospitals that follow ASHP guidelines see 18-22% lower drug costs. Generic drugs make up 90% of prescriptions but only 26% of total drug spending in the U.S. That’s the power of smart selection. It’s not perfect. There are delays, frustrations, and occasional errors. But when done right - with data, transparency, and clinical judgment at the center - the formulary system is one of the most effective tools hospitals have to deliver high-quality, affordable care.It’s not about choosing the cheapest drug. It’s about choosing the right drug - for the patient, the team, and the system.
How often are hospital formularies updated?
Most academic medical centers review their formularies every three months. Community hospitals typically do it twice a year. Updates happen when new drugs are approved, generics become available, supply issues arise, or clinical guidelines change. Urgent changes, like during a drug shortage, can be made in as little as two weeks.
Can a doctor prescribe a drug not on the formulary?
Yes, but it’s not easy. Doctors can request non-formulary drugs, but they usually need to submit a prior authorization form explaining why the formulary-approved alternatives won’t work for that patient. This process can take days, especially for specialty medications. Some hospitals require a second physician sign-off.
Why do some generic drugs look different from others?
Generic drugs must contain the same active ingredient as the brand, but they can have different fillers, coatings, or shapes. These differences can affect how fast the drug is absorbed or whether a patient can swallow it. For example, a generic tablet might be larger or harder to dissolve, which matters for elderly patients or those with swallowing difficulties. That’s why hospitals evaluate formulation, not just chemistry.
Do formularies affect patient outcomes?
Yes - when used well. Studies show hospitals with strong formulary systems have lower readmission rates, fewer medication errors, and better adherence. For example, switching to preferred generic antihypertensives has been linked to better blood pressure control. The key is consistency: when patients get the same drug every time, they’re more likely to take it correctly.
Are biosimilars included in hospital formularies yet?
Some are, but not widely. Only about 37% of U.S. hospitals have formal protocols for evaluating biosimilars. These drugs are more complex than traditional generics, so hospitals are waiting for more real-world data on long-term safety and effectiveness. Many are running pilot programs before making them standard.
How do drug shortages impact formularies?
Drug shortages are a major driver of formulary changes. In 2022, 268 generic medications faced shortages in the U.S. When one is unavailable, hospitals must quickly find an alternative - often another generic from a different manufacturer. This can lead to temporary formulary updates, staff retraining, and even medication errors. Hospitals with proactive backup plans, like Mayo Clinic’s therapeutic alternatives committee, handle these disruptions far better.


Write a comment