Autoimmune Disease & AK Risk Calculator
Estimate your risk of developing actinic keratosis based on your autoimmune condition and medications.
Quick Take
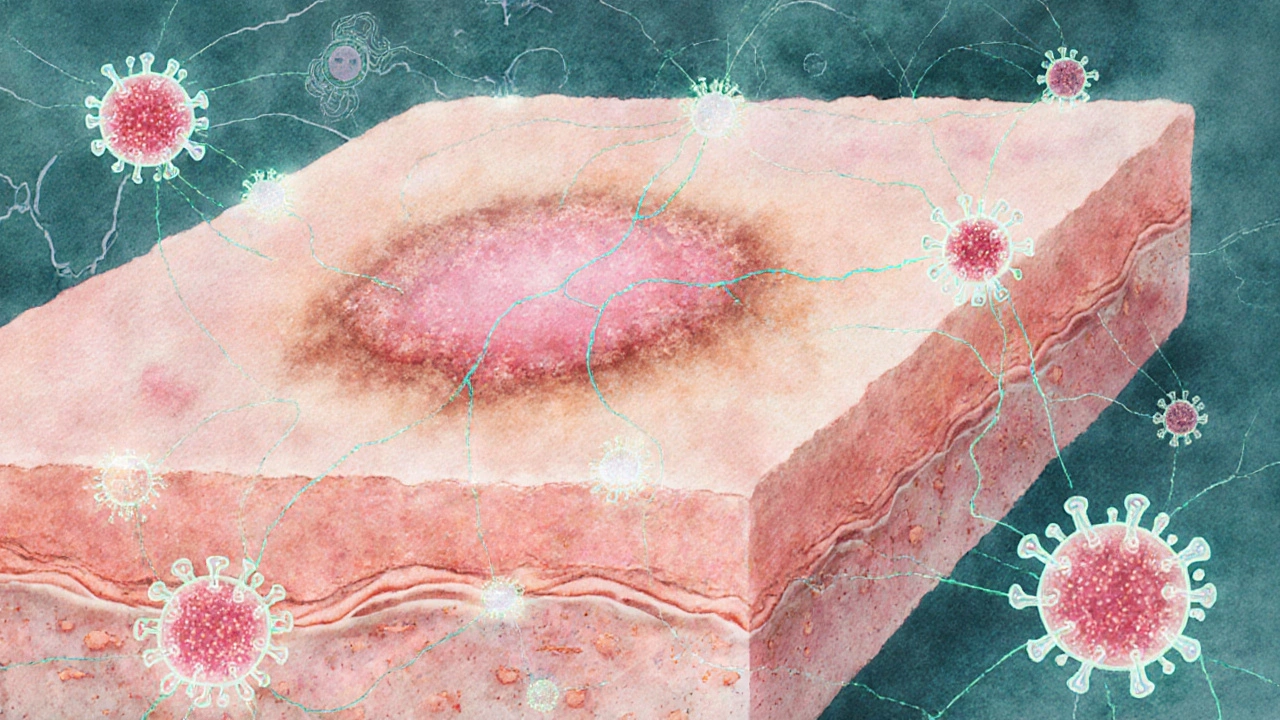
- Actinic keratosis (AK) is a sun‑induced skin lesion that can turn cancerous.
- People with autoimmune diseases show higher rates of AK than the general population.
- Chronic inflammation and immune‑system dysregulation are the main bridges between the two conditions.
- Regular skin checks and vigilant sun protection can cut the risk for anyone, especially those on immunosuppressive therapy.
What is actinic keratosis?
Actinic keratosis is a rough, scaly patch that forms on skin constantly exposed to ultraviolet (UV) radiation. It usually appears on the face, scalp, ears, forearms, and hands. Under the microscope, the epidermal cells show atypia but have not yet breached the basement membrane. If left untreated, about 1% of AK lesions each year progress to squamous cell carcinoma (SCC), the second most common non‑melanoma skin cancer.
Risk factors include fair skin, a history of sunburns, older age, and long‑term immunosuppression. Diagnosis is often clinical, but a dermatologist may perform a shave biopsy when the lesion looks atypical.
Understanding Autoimmune Diseases
Autoimmune disease refers to a group of disorders where the body’s immune system mistakenly attacks its own tissues. Common examples are systemic lupus erythematosus, rheumatoid arthritis, psoriasis, and vitiligo. These conditions share a hallmark: overactive Tcells and cytokine storms that cause chronic inflammation.
Because the immune system is constantly turned on, many patients receive immunosuppressive drugs-corticosteroids, methotrexate, biologics-that dampen protective defenses against infections and malignancies.
Shared Biological Pathways
Three core mechanisms link AK and autoimmune diseases:
- UV Radiation & DNA Damage - UV radiation induces pyrimidine dimers and other DNA lesions in skin cells. In a healthy immune system, damaged cells are cleared efficiently. In autoimmune patients, especially those on immunosuppressants, this cleanup is slower, giving mutated cells a chance to survive.
- Immune‑System Dysregulation - The immune system orchestrates surveillance for abnormal cells through Tcells, NK cells, and cytokines. Autoimmune conditions often feature an imbalance between pro‑inflammatory (Th1/Th17) and regulatory (Treg) pathways. This skewed environment can paradoxically promote tumor‑promoting inflammation while weakening anti‑tumor immunity.
- Chronic Inflammation - Persistent inflammation releases reactive oxygen species (ROS) that further damage DNA. In diseases like lupus, skin lesions already show high ROS levels, creating a perfect storm for AK development.
Evidence of an Association
Several epidemiological studies from the past decade have quantified the link:
- A 2022 cohort of 12,000 organ‑transplant recipients (a group on lifelong immunosuppression) reported a 3‑fold higher incidence of AK compared with age‑matched controls.
- A 2021 case‑control study of 2,500 patients with systemic lupus erythematosus found that 22% had at least one AK lesion, versus 8% in the general population.
- Research on psoriasis patients treated with biologics (TNF‑α inhibitors) showed a modest but significant rise in AK counts after two years of therapy.
While causation is still being untangled, the pattern is clear: immune‑modulating conditions and their treatments raise AK risk.
Clinical Implications for Patients and Providers
When a dermatologist sees a patient with an autoimmune disease, the evaluation checklist should include:
- Full skin exam focusing on sun‑exposed areas. \n
- Documentation of any existing AK lesions, noting size, thickness, and location.
- Review of immunosuppressive regimen-dose, duration, and recent changes.
- Discussion of sun‑safety habits and vitamin D supplementation (often low in these patients).
Treatment options for AK remain the same-cryotherapy, topical 5‑fluorouracil, imiquimod, or photodynamic therapy-but clinicians may opt for more aggressive management when the patient’s immune system is compromised.
Practical Tips for Reducing Risk
Even if you’re dealing with an autoimmune condition, everyday actions can keep AK at bay:
- Sun protection: Apply a broad‑spectrum sunscreen (SPF30+), reapply every two hours, and wear wide‑brim hats.
- Regular skin checks: Schedule a dermatologist visit at least annually, more often if you notice new or changing spots.
- Medication review: Talk to your rheumatologist or dermatologist about the lowest effective dose of immunosuppressants.
- Healthy lifestyle: Antioxidant‑rich foods (berries, leafy greens) may help neutralize ROS generated by chronic inflammation.
Future Directions in Research
Scientists are probing deeper into the cellular crosstalk between UV‑induced DNA damage and autoimmune inflammation. Promising avenues include:
- Targeted therapies that boost T‑cell surveillance without amplifying autoimmunity, such as checkpoint‑modulating agents.
- Genomic profiling of AK lesions from autoimmune patients to pinpoint mutation signatures unique to immunosuppressed skin.
- Long‑term prospective studies that follow newly diagnosed autoimmune patients for skin outcomes over 10‑plus years.
Understanding these pathways could eventually lead to personalized skin‑cancer prevention programs for those living with chronic immune disorders.
Comparison of Autoimmune Conditions with Reported Higher AK Prevalence
| Autoimmune Disease | Reported AK Prevalence | Key Immune Factor |
|---|---|---|
| Systemic Lupus Erythematosus | 22% | Elevated TypeI interferon |
| Psoriasis | 18% | Th17‑driven inflammation |
| Rheumatoid Arthritis | 15% | TNF‑α excess |
| Vitiligo | 13% | Auto‑reactive CD8Tcells |
| Organ‑Transplant Recipients (i.e., iatrogenic auto‑immunity) | 30% | Systemic immunosuppression |

Frequently Asked Questions
Can actinic keratosis become cancer?
Yes. While most AK lesions stay benign, about 1% transform into squamous cell carcinoma each year. Early treatment removes the risk.
Do all autoimmune diseases increase AK risk?
Not all, but many that involve chronic skin inflammation or require systemic immunosuppression show higher AK rates. Lupus, psoriasis, and rheumatoid arthritis have the strongest data.
Is sunscreen enough for someone on biologic therapy?
Sunscreen is essential but should be part of a broader plan: protective clothing, regular skin checks, and possibly lower‑dose medication under physician guidance.
Can I treat AK at home?
Over‑the‑counter options are limited. Most effective treatments-cryotherapy, prescription creams, photodynamic therapy-require a clinician’s supervision.
Should I get more frequent dermatologist visits?
If you have an autoimmune disease or take immunosuppressants, an annual full‑body skin exam is advisable. Your doctor may recommend every 6months if you have multiple AK lesions.


Write a comment