When a drug’s patent runs out, prices don’t just dip-they plummet. This isn’t speculation. It’s economics in action. In the U.S., the average price of a brand-name drug falls by 32% in the first year after patent expiration, and by 82% within eight years. That’s not a minor discount. That’s a complete overhaul of how patients pay-and how healthcare systems survive.
Why Patents Matter Before They Expire
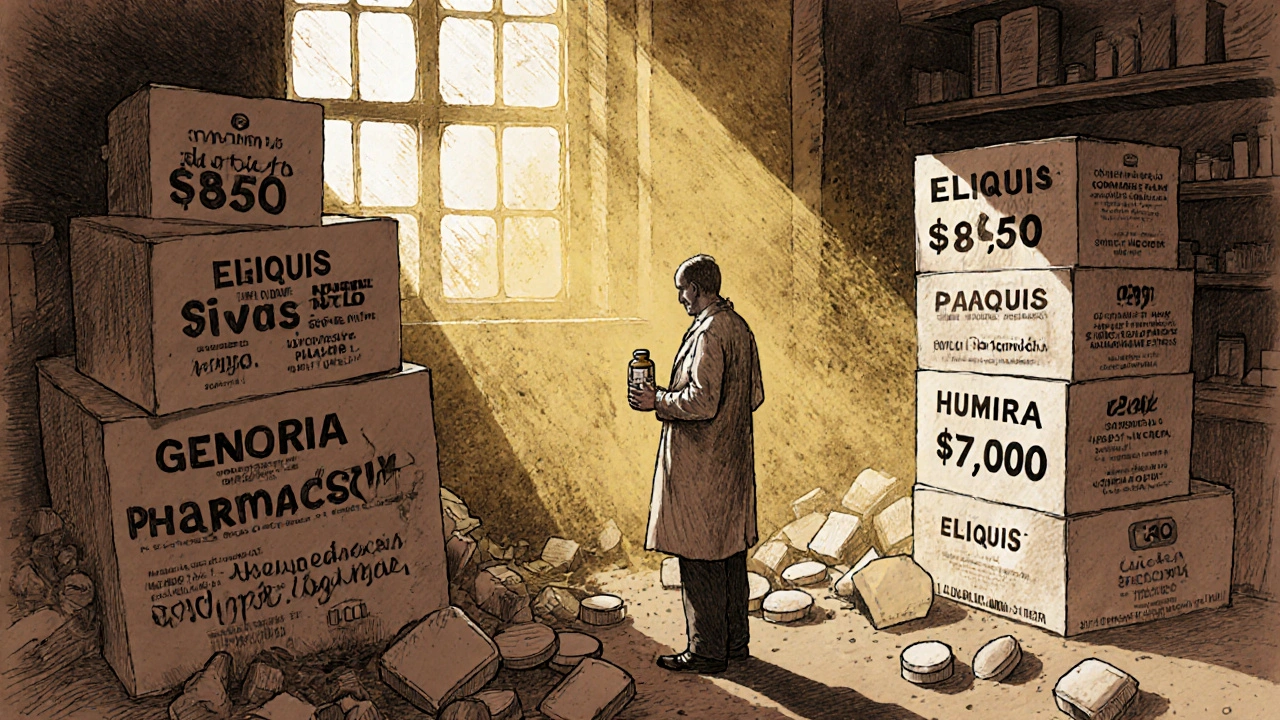
Pharmaceutical companies spend years and billions developing a new drug. To recoup that investment, they get a 20-year patent. During that time, they’re the only ones allowed to sell it. No competition. No price pressure. That’s how a drug like Eliquis can cost $850 a month. That’s how Humira hit $7,000 a dose before generics showed up. The patent system was meant to reward innovation. But over time, companies learned to stretch it. They don’t just file one patent. They file dozens-on tiny changes in dosage, packaging, or delivery method. This is called a "patent thicket." For Humira, AbbVie filed over 130 secondary patents. That kept generics out for seven years after the original patent expired. The result? Patients kept paying high prices, even when the science wasn’t new.What Happens the Day After the Patent Expires
The moment a patent expires, generic manufacturers can file to sell the same drug at a fraction of the cost. The first generic usually cuts the price by 15-20%. That’s a big deal, but it’s just the beginning. Within months, a second company enters. Then a third. By the time five or six generics are on the market, prices start to collapse. In the U.S., when 10 or more generic makers start selling the same drug, prices drop by up to 80% within three years. That’s not theory. That’s data from the NIH and the R Street Institute. Take apixaban (Eliquis). Its patent expired in 2020. Within a year, generic versions were available. Patients who paid $850 a month for the brand now pay $10. Same pill. Same effect. Just no patent protection.Why Some Drugs Don’t Drop in Price-Even After Patents Expire
Not every drug follows this pattern. Some stay expensive long after patents expire. Why? One reason: rebates and formularies. Insurance companies and pharmacy benefit managers (PBMs) don’t always choose the cheapest drug. They pick the one that gives them the biggest rebate. So even if a generic costs $5, the insurer might still cover the brand-name version at $100 because the manufacturer pays them $95 back. Patients never see the discount. This happened with Humira’s biosimilars in 2023. Multiple versions launched, yet many patients still paid $7,000 a dose. Why? Because AbbVie cut deep deals with insurers to keep Humira on top of formularies. The generics were cheaper-but locked out by contracts. Another reason: complex drugs. Biologics like Humira or insulin aren’t simple pills. They’re made from living cells. Copying them isn’t like copying aspirin. These are called biosimilars, and they take longer to approve. The FDA takes 24+ months to review them. That delays competition. And delays mean higher prices.
How the U.S. Compares to the Rest of the World
The U.S. doesn’t lead in drug affordability. It leads in drug prices. And patent expiration doesn’t fix that as quickly here as it does elsewhere. In Switzerland, prices fell just 18% over eight years after patent expiration. In the U.S., they dropped 82%. Sounds good, right? But look closer. In Europe, governments set drug prices before they hit the market. They negotiate with manufacturers. So even before a patent expires, prices are lower. When generics come in, they don’t need to crash-they just slide down gently. In the U.S., there’s no price control. So when a patent expires, the market goes wild. Prices drop hard, but only because generics flood in. And they flood in faster here-on average, generics enter 30 months after patent expiry, compared to 12-18 months in Europe. But even with faster entry, the savings don’t always reach patients.Who Benefits When Patents Expire
The biggest winners? Patients and taxpayers. A 2023 Kaiser Family Foundation survey found that 68% of insured adults saw lower out-of-pocket costs when generics became available. Medicare and Medicaid saved billions. Private insurers did too. But here’s the catch: savings don’t always show up at the pharmacy counter. If your insurance plan uses rebates, you might not feel the drop. You might still pay $50 for a drug that now costs $10 to make. That’s because the rebate goes to the insurer, not you. Pharmacists see it every day. One pharmacist in Ohio told a reporter: "I have patients who still ask why they’re paying $70 for a drug that’s been generic for three years. I explain it’s not the price-it’s their plan’s rules. They’re stunned. They think the government fixed this. They didn’t."

Write a comment