Probiotic Strain Selector for Infection Prevention
Select Your Goal
Recommended Strains
Recommended Dose
Key Considerations
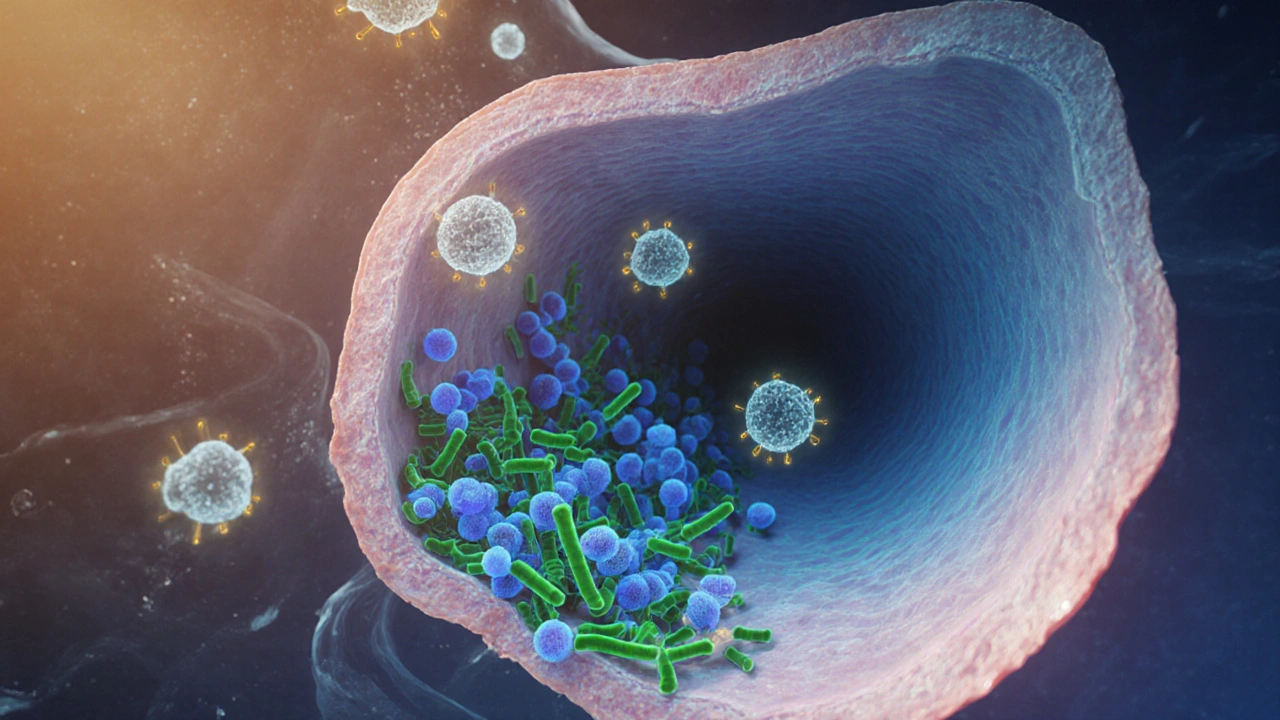
When harmful germs sneak into the body, the immune system usually steps in, but the battle can get tough if the gut environment isn’t balanced. Probiotics are live microorganisms that, when taken in adequate amounts, can tip the scales in favor of health. They work by reinforcing the gut microbiome, a bustling community that trains immune cells and keeps pathogens at bay.
Key Takeaways
- Specific probiotic strains can lower the risk of antibiotic‑associated diarrhea and certain respiratory infections.
- Benefits depend on the strain, dose, and duration of use.
- Combining probiotics with prebiotic fibers boosts their survival and activity.
- People with weakened immunity should consult a health professional before starting.
- Evidence is strongest for LactobacillusrhamnosusGG and BifidobacteriumlactisBB‑12 in infection control.
How Probiotics Influence the Immune System
The gut lining houses immune cells that patrol for invaders. When immune system receives signals from friendly microbes, it ramps up production of secretory IgA and antimicrobial peptides, creating a biochemical barrier. At the same time, probiotic bacteria compete with pathogenic bacteria for nutrients and attachment sites, a process called competitive exclusion.
Beyond crowding out bad bugs, many strains secrete substances such as lactic acid, hydrogen peroxide, and bacteriocins. These antimicrobial compounds directly inhibit the growth of harmful microbes and can even disrupt viral attachment mechanisms, adding another layer of protection.

Clinical Evidence for Infection Prevention
Antibiotic‑Associated Diarrhea (AAD)
In a 2023 meta‑analysis of 42 randomized trials, participants taking Lactobacillus strains experienced a 45% reduction in AAD compared with placebo. The most consistent results came from LactobacillusrhamnosusGG at 10billion CFU per day for the duration of antibiotic therapy.
Respiratory Tract Infections (RTI)
Another systematic review covering 19 trials found that daily intake of BifidobacteriumlactisBB‑12 lowered the incidence of colds by roughly 30% in school‑aged children. The effect was modest but statistically significant, especially when the probiotic was started at the onset of flu season.
Beyond the gut, certain strains appear to modulate lung immunity by influencing dendritic cell activity. A 2022 double‑blind study showed that adults receiving a multi‑strain blend (including Lactobacilluscasei and Bifidobacteriumbreve) reported fewer days with fever and cough during a winter outbreak.
Choosing the Right Strain and Dose
Not all probiotics are created equal. When targeting infection prevention, look for strains that have been investigated in human trials for that specific outcome. Below is a quick reference.
| Strain | Typical Dose (CFU) | Primary Benefit |
|---|---|---|
| Lactobacillus rhamnosus GG | 1‑10×10⁹ | Reduces antibiotic‑associated diarrhea |
| Bifidobacterium lactis BB‑12 | 1‑5×10⁹ | Lowers incidence of common colds |
| Lactobacillus casei Shirota | 5‑10×10⁹ | Supports respiratory tract immunity |
| Bifidobacterium breve BR03 | 2‑8×10⁹ | Shortens duration of flu‑like symptoms |
For most healthy adults, adding probiotics to the daily routine is a low‑risk strategy to support infection resistance.

Practical Tips for Incorporating Probiotics
Timing matters: take the supplement with a meal that contains some fat, as many bacterial cells are more resilient in that environment. If you prefer foods, fermented options such as kefir, sauerkraut, and kimchi can provide a natural dose.
Pairing with prebiotics-non‑digestible fibers found in bananas, onions, and chicory root-feeds the beneficial bacteria and helps them colonize the gut more effectively.
Store capsules according to the manufacturer’s instructions; some require refrigeration, while many newer strains are shelf‑stable thanks to freeze‑drying technologies.
Safety Considerations and Who Should Seek Advice
Probiotics are safe for the vast majority of people, but individuals who are immunocompromised or have a central venous catheter should talk to their doctor before starting, as rare cases of bloodstream infection have been reported.
Those with a history of small intestinal bacterial overgrowth (SIBO) might experience bloating when beginning a high‑dose regimen; a gradual increase can mitigate discomfort.
Always choose products that list the strain name, CFU count at expiration, and have third‑party testing to ensure quality.
Frequently Asked Questions
Can I get the same benefits from fermented foods as from supplements?
Fermented foods do contain live cultures, but the strains, amounts, and survivability vary widely. Supplements let you target specific strains with proven doses, while foods are great for daily variety and added nutrients.
How long should I take a probiotic to see infection‑prevention effects?
Most studies show benefits after 2‑4 weeks of daily use. For antibiotic‑associated diarrhea, start the probiotic at the same time as the antibiotic and continue for at least one week after finishing the course.
Do all probiotic capsules need refrigeration?
Not anymore. Many manufacturers use freeze‑drying and protective coatings that keep the bacteria viable at room temperature. Check the label; if it says “keep refrigerated,” follow that instruction.
Can probiotics interact with medications?
Generally no major interactions, but some immunosuppressive drugs may alter how the gut microbiome responds. If you’re on such medication, discuss probiotic use with your physician.
What dose of Lactobacillus rhamnosus GG is effective for preventing diarrhea?
Clinical trials most often used 1‑10×10⁹ colony‑forming units (CFU) per day, taken with food, throughout the antibiotic course and a few days beyond.

Write a comment