Ulcer-Friendly Food Checker
Is This Food Ulcer-Friendly?
Check if your food choices are safe for stomach ulcers based on medical recommendations. Select from common foods or type your own.
Enter a food name to see if it's ulcer-friendly.
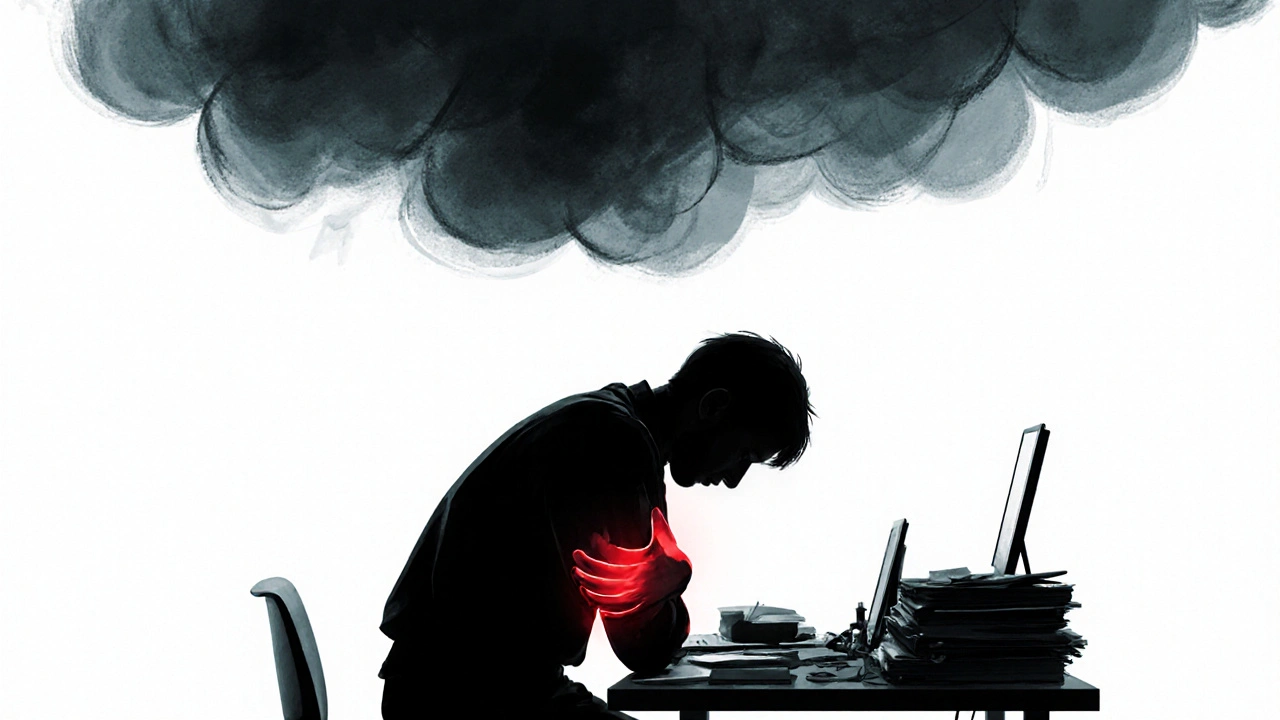
When stress and a stomach ulcer team up, the pain can feel relentless and the whole day seems off‑balance. The good news? Most of the flare‑ups are within your control. By understanding how stress fuels ulcer pain and applying a mix of lifestyle tweaks, diet choices, and simple medical aids, you can calm the burn and get back to normal.
What Exactly Is a Stomach Ulcer?
Stomach ulcer is a sore that forms on the lining of the stomach, technically a type of peptic ulcer. It develops when the protective mucus layer is weakened and stomach acid eats into the tissue, creating a raw spot that can bleed or scar. Common causes include infection with Helicobacter pylori, frequent use of NSAIDs (like ibuprofen), and chronic stress.
Symptoms range from a gnawing ache after meals to nausea, bloating, and occasional dark stools. While many ulcers heal on their own, untreated cases can lead to complications such as perforation or bleeding.
How Stress Turns Up the Heat
Stress is the body’s response to perceived threats, releasing hormones like cortisol. Elevated cortisol can increase stomach acid production and slow the regeneration of the mucosal lining, making an existing ulcer more painful.
Beyond hormones, stress often changes habits: you might skip meals, reach for coffee, or over‑use NSAIDs for headache relief. Each of these pushes the ulcer’s environment toward irritation.
Core Lifestyle Adjustments
- Eat on a schedule. Aim for small, balanced meals every 3‑4 hours to keep acid levels steady.
- Limit alcohol and caffeine. Both stimulate acid secretion.
- Quit smoking. Nicotine hampers mucus production and blood flow to the stomach lining.
- Stay hydrated. Water dilutes gastric acid and supports healing.

Ulcer‑Friendly Diet - What to Choose and What to Skip
Food isn’t a magic cure, but certain choices can soothe the lining while others aggravate it.
Best picks include:
- Low‑fat dairy such as yogurt (contains probiotics that help balance the gut microbiome).
- Lean proteins - chicken, fish, tofu - prepared without heavy frying.
- Whole grains like oatmeal and brown rice that are gentle on the stomach.
- Non‑citrus fruits (bananas, melons) and cooked veggies (carrots, zucchini).
Foods to avoid:
- Spicy peppers and hot sauces - they can irritate the ulcer surface.
- Acidic fruits (oranges, tomatoes) and fruit juices.
- Chocolate and mint - both can relax the lower esophageal sphincter, letting acid rise.
- Fried or overly greasy meals that delay stomach emptying.
Medical Tools That Calm the Burn
When lifestyle alone isn’t enough, short‑term medication bridges the gap while the ulcer heals.
| Medication Type | How It Works | Typical Use | Key Considerations |
|---|---|---|---|
| Antacid | Neutralizes existing stomach acid | Fast relief, taken after meals | Provides short‑term relief only; overuse can cause alkalosis |
| H2 Blocker | Blocks histamine receptors, reducing acid output | Taken twice daily, works within an hour | Less potent than PPIs; may develop tolerance |
| Proton Pump Inhibitor | Inhibits the final step of acid production | Once‑daily, usually before breakfast | Most effective for healing; long‑term use linked to nutrient malabsorption |
Doctors often start with a Proton Pump Inhibitor (PPI) like omeprazole for 4‑8 weeks, then taper based on healing progress seen in an endoscopy.
Stress‑Reduction Practices That Really Work
Targeting the stress‑ulcer loop means calming both mind and body. Here are evidence‑backed options you can try at home:
- Deep‑breathing exercises: Inhale for 4seconds, hold 7, exhale 8. Repeat five minutes twice a day. Controlled breathing lowers cortisol and slows acid secretion.
- Progressive muscle relaxation: Tense each muscle group for 5seconds, then release. A 10‑minute session before bed can cut night‑time acid spikes.
- Mindful walking: A 20‑minute walk at a comfortable pace, paying attention to each step, reduces the fight‑or‑flight response.
- Yoga or tai chi: Gentle flows focusing on the diaphragm improve gastric motility. A study from the University of Auckland (2023) showed a 30% drop in ulcer pain scores after six weeks of thrice‑weekly yoga.

When to Call a Healthcare Professional
If you notice any of these signs, seek medical attention promptly:
- Vomiting blood or material that looks like coffee grounds.
- Black, tarry stools (possible bleeding).
- Sudden, severe abdominal pain that doesn’t improve with antacids.
- Weight loss or loss of appetite lasting more than two weeks.
Early diagnosis-often via endoscopy-helps prevent serious complications and allows tailored treatment, such as eradication therapy for Helicobacter pylori.
Quick Checklist - Your Daily Ulcer‑Stress Defense
- Take prescribed medication with water, not with coffee.
- Eat a balanced, low‑acid breakfast within an hour of waking.
- Practice a 5‑minute breathing routine before meals.
- Avoid NSAIDs unless a doctor says it’s safe.
- Log stress triggers; notice patterns that worsen pain.
Frequently Asked Questions
Can stress alone cause a stomach ulcer?
Stress by itself rarely creates an ulcer, but it raises stomach acid and weakens the mucus barrier, making existing ulcers worse. Combined with factors like H.pylori infection or NSAID use, stress becomes a significant aggravator.
Are over‑the‑counter antacids enough for long‑term relief?
Antacids neutralize acid quickly but don’t prevent new acid from being produced. They’re useful for occasional flare‑ups, but persistent ulcers need acid‑suppressing drugs like H2 blockers or PPIs, plus addressing the underlying cause.
How long does it take for a stomach ulcer to heal?
With proper medication and lifestyle changes, most uncomplicated ulcers heal in 4-8 weeks. Follow‑up endoscopy may be recommended to confirm healing, especially for larger lesions.
Is it safe to use ibuprofen if I have a stomach ulcer?
Generally no. Ibuprofen and other NSAIDs inhibit prostaglandins that protect the stomach lining, worsening ulcers. If pain relief is needed, ask a doctor about acetaminophen or a prescribed ulcer‑friendly analgesic.
Can diet alone cure a stomach ulcer?
Diet helps manage symptoms and supports healing but rarely cures an ulcer on its own. Eradicating H.pylori (if present) and reducing acid with medication are usually necessary for full recovery.

Write a comment