Every year, more than 100,000 people in the U.S. are diagnosed with invasive melanoma-the most dangerous form of skin cancer. But here’s the truth: melanoma is also one of the most preventable cancers if you know what to look for and how to act. Unlike other skin cancers, melanoma spreads fast. Left undetected, it can move from your skin to your lymph nodes, lungs, liver, or brain. But caught early? The chance of surviving five years or more is over 99%. That’s not a guess. That’s data from the Surveillance, Epidemiology, and End Results (SEER) Program. This isn’t about fear. It’s about awareness, action, and knowing exactly what to do before it’s too late.
What Melanoma Really Is (And Why It’s Different)
Melanoma starts in melanocytes, the cells that give your skin its color. When these cells get damaged-usually by UV radiation from the sun or tanning beds-they can turn cancerous. It doesn’t always look like a dark mole. Sometimes it’s pink, red, or even flesh-colored. That’s why people with darker skin often get diagnosed later: doctors and patients alike miss it because they’re looking for the classic black spot.
There are four main types:
- Superficial spreading melanoma (70% of cases): The most common. It grows sideways across the skin before going deeper.
- Nodular melanoma (15-30%): Grows fast and sticks up. Often dark, but can be colorless. This one doesn’t follow the usual mole rules.
- Lentigo maligna melanoma (10-15%): Usually on sun-exposed skin like the face or arms in older adults. Starts as a flat, irregular patch.
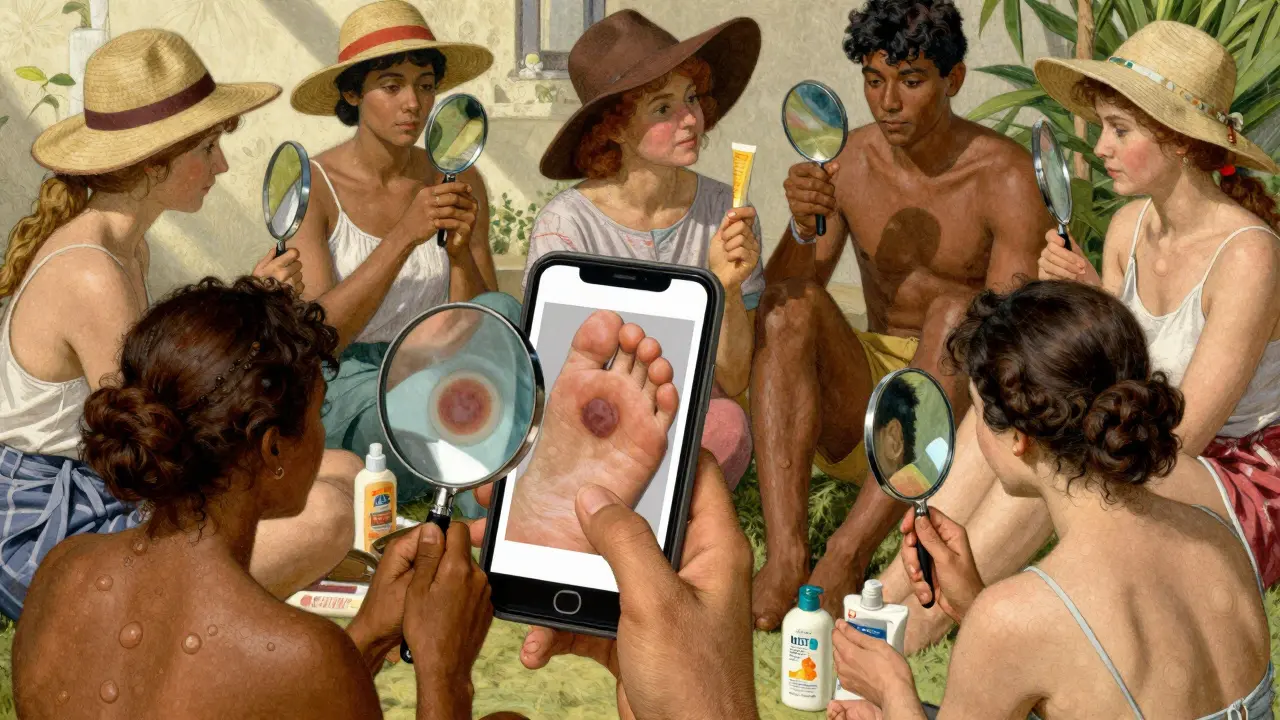
- Acral lentiginous melanoma (2-8%): Found on palms, soles, or under nails. More common in people with darker skin. Often mistaken for bruises or dirt.
What makes melanoma deadly isn’t how common it is-it’s how fast it spreads. It makes up only 1% of skin cancers but causes the most deaths. And it’s rising. In 2025, there will be over 104,960 new invasive cases in the U.S. That’s up 5.9% from last year. The good news? Most of these cases are preventable.
How to Prevent Melanoma Before It Starts
Over 90% of melanomas are linked to UV exposure. That means your daily choices matter more than you think. Sunscreen alone won’t save you. You need a full strategy.
- Wear broad-spectrum SPF 30+ every day-even when it’s cloudy. UVA rays penetrate clouds and glass. A 2023 study showed daily sunscreen use cuts melanoma risk by 40% over 10 years.
- Avoid tanning beds completely. People who use them before age 35 increase their melanoma risk by 75%. The FDA and CDC both call indoor tanning a public health crisis.
- Seek shade between 10 a.m. and 4 p.m. That’s when UV rays are strongest. Even under an umbrella, up to 80% of UV radiation can reach you.
- Wear UPF 50+ clothing, wide-brimmed hats, and UV-blocking sunglasses. Regular cotton shirts only block about 50% of UV. Specialized sun-protective fabrics are worth the investment.
- Check the UV index daily. Apps like QSun’s UV Index now integrate with weather forecasts. If the index is 6 or higher, take extra precautions.
And don’t assume you’re safe because you don’t burn. People with darker skin tones are less likely to burn, but they’re more likely to die from melanoma because it’s found later. Prevention isn’t just for fair-skinned people. It’s for everyone.
How to Detect Melanoma Early: The ABCDE Rule and Beyond
Early detection saves lives. The five-point ABCDE checklist is still the gold standard:
- Asymmetry: One half doesn’t match the other.
- Border: Edges are ragged, blurred, or notched.
- Color: More than one color-black, brown, tan, red, white, or blue.
- Diameter: Larger than 6mm (about the size of a pencil eraser). But some melanomas are smaller.
- Evolving: Changing in size, shape, color, or texture. Or developing new symptoms like itching, bleeding, or crusting.
But here’s what most people miss: new spots and ugly ducklings. An ugly duckling is a mole that looks different from all the others on your body. That’s the one to check. And don’t ignore new moles after age 30. Most melanomas appear as new growths, not changes in existing moles.
Self-exams should take 10-15 minutes, once a month. Do them after a shower, in good lighting. Use a mirror for hard-to-see areas-back, scalp, between toes, under nails. Take photos of suspicious spots with your phone to track changes. Many patients on patient forums say their diagnosis came from noticing a spot that “just didn’t look right.”
For high-risk people-those with more than 50 moles, a family history of melanoma, or a past skin cancer-professional skin exams every 3 to 6 months are recommended. But wait times are long. The average wait for a dermatologist is nearly 29 days. In rural areas, it’s over two months. That’s why teledermatology is growing. Apps and platforms like DermEngine now offer AI-assisted analysis. One 2025 FDA-approved tool, VisualizeAI, detects melanoma with 93.2% accuracy. It’s not a replacement for a doctor, but it’s a powerful early warning system.
How Melanoma Is Treated-By Stage
Treatment depends entirely on how far the cancer has spread. There’s no one-size-fits-all approach.
Stage 0 (In Situ)
The cancer is only in the top layer of skin. Surgery to remove the spot with a small margin (0.5-1 cm) is usually all that’s needed. Cure rate: nearly 100%.
Stage I-II (Localized)
The tumor has grown deeper but hasn’t spread to lymph nodes. Treatment: wider surgical removal (1-2 cm margins). For tumors over 0.8 mm thick, doctors often recommend a sentinel lymph node biopsy (SLNB)-a minor procedure to check if cancer has moved to nearby lymph nodes. If negative, no further treatment is needed. Five-year survival: 97% for Stage IA, still over 90% for Stage IIB.
Stage III (Regional Spread)
Cancer has reached nearby lymph nodes or tiny satellite tumors. Surgery is still the first step, but now it’s followed by adjuvant therapy. That means drugs like nivolumab, pembrolizumab, or ipilimumab to kill any hidden cancer cells. These are immunotherapies-medicines that help your immune system fight cancer. Side effects can be serious, but they’re far less than they were a decade ago. Five-year survival: around 70-80%.
Stage IV (Metastatic)
Cancer has spread to distant organs. This is where things get complex. Treatment options include:
- Immunotherapy: Drugs like nivolumab + ipilimumab. In the CheckMate 067 trial, 52% of patients were still alive five years later. That’s a massive jump from just 10% in 2010.
- Targeted therapy: For patients with BRAF mutations (about half of all melanomas). Dabrafenib + trametinib can shrink tumors quickly, with a median survival of 34 months. But resistance often develops.
Doctors now test every Stage IIB-IV patient for BRAF, NRAS, KIT, and NF1 mutations. That’s because treatment depends on your tumor’s genetics. There’s no point giving a BRAF drug if your cancer doesn’t have the mutation.
Cost is a huge barrier. A single infusion of nivolumab can cost $15,000-$20,000. Even with insurance, out-of-pocket costs can hit $28,000 per year. That’s why so many patients on Reddit talk about financial toxicity. It’s not just about survival-it’s about staying financially alive.
What’s New in 2025: Breakthroughs That Are Changing Outcomes
The last five years have been the most exciting in melanoma history.
In early 2025, the FDA approved two major advances:
- DermEngine’s VisualizeAI: The first AI tool cleared for melanoma detection. It analyzes dermoscopy images and flags suspicious lesions with 93.2% accuracy. Hospitals and clinics are rolling it out now.
- mRNA-4157/V940: A personalized cancer vaccine made from your tumor’s unique mutations. When paired with pembrolizumab, it cut recurrence risk by 44% in Stage IIB-IV patients. It’s not a cure yet, but it’s a game-changer for preventing relapse.
The CDC is also launching a $28.5 million push to integrate real-time UV index alerts into weather apps. By 2026, over 120 million Americans could get daily warnings on their phones. That’s prevention at scale.
And teledermatology kiosks are now being installed in 150 Walmart health clinics across rural states. No appointment needed. Just walk in, take photos of your skin, and get a dermatologist’s assessment within 48 hours. It’s not perfect-but it’s better than waiting three months.

Who’s at Risk-and Why It’s Not Just About Fair Skin
Yes, fair skin, blue eyes, red hair, and lots of sunburns raise your risk. But melanoma doesn’t play favorites.
Black patients make up only 2% of all melanoma cases, but 12% of advanced cases on patient forums. Why? Because melanoma often shows up on the palms, soles, or under nails-areas doctors and patients don’t check. One patient, DJohnson_MD, was told his foot lesion was a bruise for over a year. By the time he got a biopsy, it was Stage III.
Older women are another growing concern. While melanoma rates are dropping in young adults, they’re rising 3% a year in women over 60. Why? Decades of sun exposure, plus thinner skin and less awareness.
And don’t forget: if you’ve had one melanoma, your risk of a second one is 8-10 times higher. Lifelong monitoring isn’t optional-it’s essential.
What You Can Do Right Now
You don’t need a medical degree to save your life. Here’s your action plan:
- Do a monthly skin self-check using the ABCDE rule. Take photos of anything new or changing.
- Use sunscreen every day-even indoors near windows.
- Never use tanning beds. There’s no safe level.
- Know your risk: Family history? More than 50 moles? Past sunburns? If yes, see a dermatologist every 6 months.
- Ask for a full-body skin exam during your annual check-up. Don’t wait for symptoms.
- Download a UV index app and check it daily. If it’s 6 or higher, cover up.
Melanoma isn’t a death sentence anymore. It’s a warning sign-and if you respond quickly, it’s a chance to live a long, healthy life. The tools are here. The knowledge is out there. Now it’s up to you to use them.

Write a comment