Childhood Parkinsonism Medication Dosage Calculator
Levodopa/Carbidopa Dosage Calculator
Calculate appropriate dosage ranges based on child's weight. This is for informational purposes only.
Recommended Dosage Range
Note: Medication dosages should be determined by a qualified healthcare provider. This calculator is for informational purposes only and does not replace professional medical advice.
When Parkinsonism is diagnosed in a child or teenager, the ripple effects reach far beyond motor symptoms. Families suddenly find themselves navigating a medical maze, schools adjust schedules, and friends try to understand a condition they thought only adults got.
Parkinsonism children face a unique blend of challenges that demand tailored information and support.
Understanding Parkinsonism in Young People
Juvenile Parkinsonism (often called early‑onset Parkinsonism) refers to cases that appear before the age of 21. While the underlying biology mirrors adult Parkinson's disease-loss of dopamine‑producing neurons and the buildup of Lewy bodies-the timeline, genetics, and daily impact differ markedly.
The core driver, Dopamine, is a brain chemical that fine‑tunes movement, mood, and cognition. In kids, dopamine depletion can interfere with learning, play, and social development, making early detection crucial.
Core Motor and Non‑Motor Symptoms
Motor signs often look familiar: tremor, stiffness, and slowed movements. However, youngsters may display these in ways that blend into typical adolescence. For example, a teenager’s “shaky handwriting” might be dismissed as nerves, while a younger child could appear clumsy during playground games.
Non‑motor symptoms can be even more disruptive. Sleep disturbances, constipation, and mood swings are common, but they may be misattributed to stress or hormonal changes. Recognizing these cues early can prevent a cascade of secondary issues such as anxiety or academic decline.
Why the Disease Differs in Kids vs. Adults
Three key factors set juvenile cases apart:
- Genetics: Up to 30% of early‑onset cases link to specific Genetic mutation families, such as PARK2 (parkin) or PINK1. These inherited forms often progress slower but can start at a very young age.
- Brain Plasticity: A child’s nervous system is still wiring itself. This can mask some symptoms while amplifying others, like difficulty with fine motor tasks (tying shoes, using utensils).
- Life Stage: School, sports, and peer relationships are central to identity. Any disruption hits harder emotionally than it might for an adult whose routines are already established.
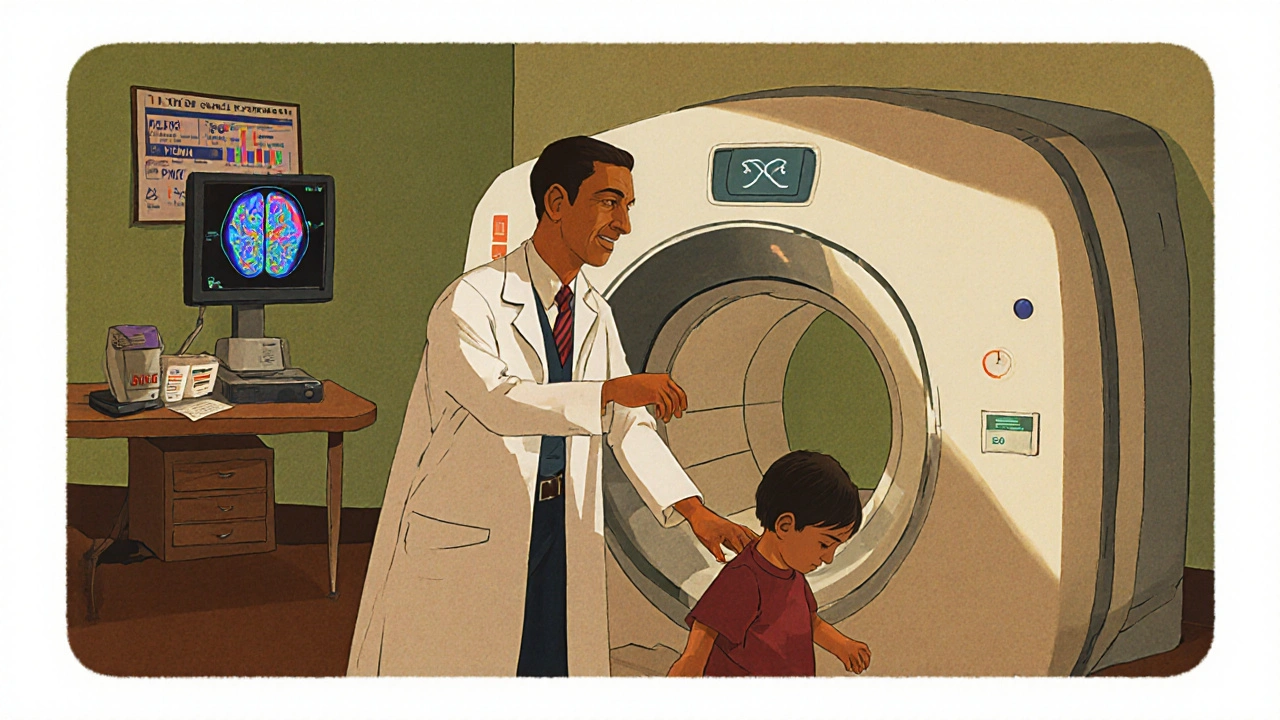
Diagnosis and Common Tests
Because symptoms overlap with typical childhood conditions, a thorough evaluation is essential. Pediatric neurologists usually combine the following:
- Clinical exam focusing on gait, reflexes, and tremor patterns.
- Brain imaging (MRI) to rule out structural issues.
- DaTscan (dopamine transporter imaging) - though less common in children, it can confirm dopamine loss.
- Genetic testing when a family history or early onset raises suspicion.
Neurodevelopmental assessments help chart how the disorder affects learning and attention, guiding school‑based interventions.
Treatment Options: Medication, Therapy, Surgery
Medication remains the frontline approach, but dosing must consider a child’s growth and metabolism.
| Drug | Typical Dose (Kids) | Typical Dose (Adults) |
|---|---|---|
| Levodopa/Carbidopa | 0.5‑1 mg/kg three times daily | 300‑600 mg daily |
| Rasagiline | Not routinely used | 1 mg daily |
| Pramipexole | 0.125‑0.25 mg three times daily | 0.5‑1.5 mg three times daily |
Beyond drugs, Physical therapy targets strength, balance, and coordination. Tailored exercises help kids keep up with peers and reduce fall risk.
When medication stops providing adequate control, Deep brain stimulation (DBS) may be considered, even for teenagers. DBS involves implanted electrodes that modulate abnormal brain signals, offering smoother motor function and lower medication doses.
Managing Daily Life: School, Sports, Family Support
Success in school often hinges on practical accommodations:
- Extended time on tests to account for slower writing speed.
- Allowing the use of a laptop or speech‑to‑text software for note‑taking.
- Physical‑education modifications-like low‑impact activities-to keep the child active without over‑exertion.
Coaching staff should be aware of medication timing to avoid “off‑period” fatigue during practice. Parents benefit from Family counseling, which addresses the emotional strain of chronic illness and equips siblings with coping tools.
Peer education programs can demystify the condition, reducing stigma and fostering inclusive friendships.
Outlook and Future Research
Thanks to early diagnosis and multidisciplinary care, many children with juvenile Parkinsonism lead active, fulfilling lives well into adulthood. Ongoing research into gene‑editing therapies and novel dopamine‑mimicking compounds holds promise for disease‑modifying treatments.
Clinicians are also studying neuroprotective strategies-like exercise‑induced brain‑derived neurotrophic factor (BDNF) release-to slow progression from the youngest ages.
What are the first signs of Parkinsonism in children?
Early signs often include a subtle tremor in the hands, stiffness that makes dressing difficult, and slower handwriting. Non‑motor clues such as frequent constipation or disrupted sleep can also be early red flags.
How is juvenile Parkinsonism diagnosed differently from adult Parkinson's disease?
Doctors combine a neurological exam with genetic testing, growth‑adjusted imaging, and neurodevelopmental assessments. Because children may not report symptoms clearly, clinicians rely more on parental observations and school reports.
Can medication doses be the same for kids and adults?
No. Doses are weight‑based and adjusted for metabolism. For example, levodopa is typically started at 0.5‑1 mg per kilogram three times daily, far lower than adult standards.
Is deep brain stimulation safe for teenagers?
When performed by an experienced team, DBS is considered safe for carefully selected teens. It can reduce medication needs and improve motor control, but long‑term monitoring is essential.
What role does physical therapy play in managing the condition?
Physical therapy strengthens muscles, enhances balance, and teaches strategies to overcome stiffness. Regular sessions can keep a child active in sports and daily life, reducing fall risk and improving confidence.

Write a comment