Every year, tens of thousands of people end up in the emergency room because they didn’t realize they were taking the same medicine twice. Not because they were careless, but because they didn’t know that their prescription painkiller and their store-brand cold medicine had the exact same active ingredient. This isn’t rare. It’s common. And it’s preventable.
What Are Double Ingredients?
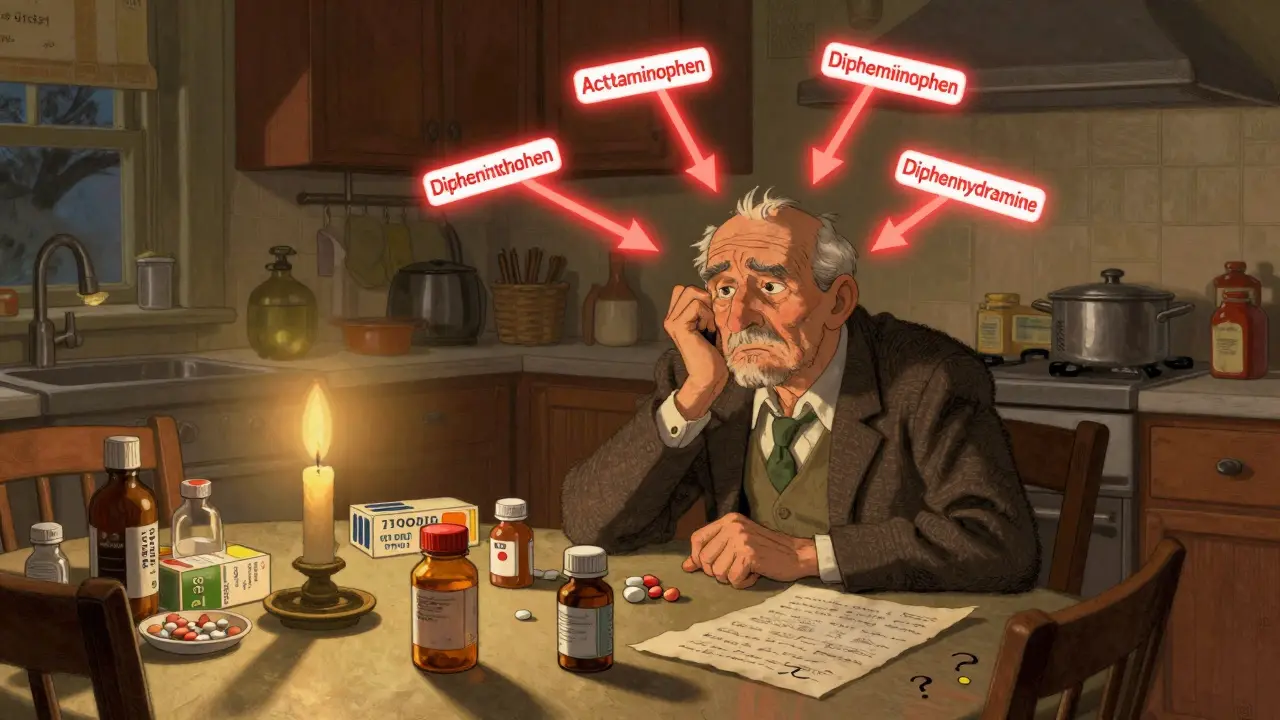
Double ingredients happen when you take two or more medications that contain the same active drug. It sounds simple, but it’s easy to miss. You might be taking a prescription medication for pain, and then reach for an OTC cold tablet because you’ve got a stuffy nose. Both might contain acetaminophen. You don’t think twice-until your liver starts to fail. The most dangerous combinations involve acetaminophen, NSAIDs like ibuprofen, sedatives like diphenhydramine, and stimulants like pseudoephedrine. These ingredients show up everywhere: pain relievers, sleep aids, cold and flu remedies, allergy pills, even some herbal supplements. The problem isn’t just the number of pills you take-it’s that you don’t know what’s inside them.Why This Happens More Than You Think
About 40% of adults over 65 take five or more medications regularly. That’s called polypharmacy. And for nearly a third of them, at least one of those medications overlaps with another in active ingredients. The CDC says older adults make up 65% of hospitalizations from these errors. But it’s not just seniors. Anyone managing multiple conditions-diabetes, high blood pressure, arthritis, depression-is at risk. Here’s why it’s so easy to slip up:- Prescription labels rarely mention what’s in OTC products.
- OTC drug labels use confusing names. Tylenol, Panadol, Excedrin, and store-brand pain relievers all have acetaminophen-but you won’t see that word on the front.
- People don’t tell doctors about OTCs or supplements. One study found 68% of patients hide their use of herbal remedies or OTC meds.
- Many patients use multiple pharmacies. If you fill prescriptions at CVS, Walgreens, and a local clinic, none of them talk to each other.
The Real Danger: How Much Is Too Much?
Acetaminophen is the #1 cause of accidental overdose in the U.S. The NIH reports 56,000 ER visits every year from it. The safe daily limit is 3,000 to 4,000 milligrams-but most people don’t know that. A single Extra Strength Tylenol tablet has 500 mg. A Vicodin tablet has 325 mg. A cold tablet might have another 325 mg. Do the math: three pills a day from different sources can hit 2,000 mg before lunch. By bedtime, you’re over the limit. Sedatives are another silent killer. Diphenhydramine (Benadryl, Unisom, Tylenol PM) makes you drowsy. So does hydroxyzine (prescription), doxylamine (NyQuil), and even some antihistamines labeled "non-drowsy"-because they wear off at night. Mix them, and you risk slowed breathing, confusion, falls, or even coma. NSAIDs like ibuprofen and naproxen are no safer. Taking Advil for your knee pain and Aleve for your headache? That’s two full daily doses. Add a prescription NSAID like celecoxib? You’re asking for stomach bleeding or kidney damage.
Who’s Most at Risk?
It’s not just seniors. But they’re the most vulnerable. Why? Because they’re more likely to:- See multiple specialists (cardiologist, rheumatologist, neurologist) who each prescribe without knowing what the others ordered.
- Use OTC meds for chronic symptoms like sleeplessness or joint pain.
- Have memory issues or take meds in bulk without checking labels.
How to Protect Yourself
The good news? 89% of these errors can be prevented with simple steps. Here’s how:- Make a complete list of everything you take. Not just prescriptions. Include OTC pills, vitamins, herbal teas, gummies, eye drops, creams, and patches. Write down the name, dose, and how often you take it.
- Keep this list with you. In your wallet. In your phone notes. On your fridge. Update it every time you start or stop something.
- Use one pharmacy. Filling all your meds at one pharmacy-whether it’s CVS, Walgreens, or a local independent-lets their system flag duplicates. Studies show this cuts double ingredient errors by 63%.
- Ask your pharmacist. When you pick up a new prescription, ask: "Could this interact with anything else I’m taking?" Pharmacists catch 87% of potential issues during medication reviews.
- Ask your doctor. At every appointment, say: "I’m taking [list]. Is anything here overlapping?" Don’t wait for them to ask. They rarely do.
- Check OTC labels like a detective. Look for the "Drug Facts" panel. The active ingredients are listed right under the title. If you see acetaminophen, diphenhydramine, or ibuprofen, cross-check your prescription list.
- Review your meds yearly. Set a calendar reminder. Once a year, sit down with your list and go through each item. Ask: "Do I still need this?" "Is there a safer alternative?"
What’s Being Done to Fix This
The system is catching up. Since 2020, the FDA has required all OTC products to use a standardized "Drug Facts" label that clearly lists active ingredients. By 2025, every product must follow this format. That’s a big step. Electronic health records now have "double ingredient check" tools. Epic and Cerner systems alert doctors if a new prescription overlaps with a patient’s OTC meds-when those meds are entered. But here’s the catch: only 43% of systems actually track OTC use. If you don’t tell them, they won’t know. The Pharmacy Quality Alliance now requires Medicare Part D plans to screen for drug interactions. Since 2021, this has reduced hospitalizations from double ingredients by 28% among seniors. Apple Health and other smartphone apps now flag duplicate ingredients. If you log your meds in Apple Health, it will warn you if you’re about to take two things with acetaminophen. It’s not perfect-but it’s a start.Real Stories, Real Consequences
One Reddit user, "MedSafety101," shared how they took three different cold medicines-all with pseudoephedrine-because they thought each was "different." They ended up in the ER with a blood pressure spike of 210/110. Another patient at UCLA Health took Vicodin and a store-brand cold tablet for weeks. She didn’t know both had acetaminophen. By the time she was hospitalized, her liver enzymes were through the roof. She needed a transplant. These aren’t outliers. They’re examples of what happens when we assume the medicine we buy at the drugstore is "safe" because it’s not prescription.Final Advice
You don’t need to be a pharmacist to keep yourself safe. You just need to be curious. Ask questions. Write things down. Don’t assume. If you’re taking more than three medications, you’re at risk. If you’re taking OTCs, you’re at risk. If you’re seeing multiple doctors, you’re at risk. The system isn’t perfect. But you are your own best defense. Keep your list. Use one pharmacy. Talk to your pharmacist. Ask your doctor. Check the label. One small habit could save your liver-or your life.Can I take OTC pain relievers with my prescription pain meds?
Only if you know what’s in both. Many prescription painkillers like Vicodin, Percocet, and tramadol already contain acetaminophen. Adding Tylenol, Advil, or a cold medicine with acetaminophen can push you over the safe daily limit. Always check the active ingredients on the label. If both contain the same drug, don’t take them together.
Why don’t doctors always catch this?
Most electronic health records don’t include OTC medications unless the patient reports them. Doctors are trained to focus on prescriptions and diagnoses, not what you bought at the drugstore. A 2022 study found that 45% of prescription labels don’t even mention OTC overlaps. If you don’t tell them, they can’t help you.
Is it safe to take multiple OTC cold medicines at once?
No. Cold medicines often combine multiple ingredients: pain relievers, decongestants, antihistamines, and cough suppressants. Taking two different brands means you’re doubling up on at least one of them. For example, DayQuil and NyQuil both contain acetaminophen and dextromethorphan. Even if you space them out, you’re still building up toxic levels. Stick to one product and read the label carefully.
What should I do if I think I’ve taken too much of an ingredient?
If you suspect an overdose-especially with acetaminophen or sedatives-call Poison Control at 1-800-222-1222 immediately. Don’t wait for symptoms. Liver damage from acetaminophen can happen without pain or nausea until it’s too late. For sedatives, watch for extreme drowsiness, confusion, slow breathing, or unresponsiveness. Go to the ER if you’re unsure.
Can I use a medication app to track my drugs?
Yes, and it’s one of the best tools you can use. Apps like Medisafe, MyTherapy, and Apple Health let you log all your meds-including OTCs and supplements. Many will warn you about duplicate ingredients, interactions, and missed doses. Just make sure you enter everything accurately, including doses and frequencies. These apps are not perfect, but they’re far better than relying on memory.

Write a comment